Prevalence and Gastric Location of Helicobacter pylori in Patients with Intestinal Atrophy and Metaplasia in a Tertiary Care Institution in Colombia
DOI:
https://doi.org/10.22516/25007440.858Keywords:
Helicobacter pylori, Gastric atrophy, Intestinal metaplasia, Gastric cancer, Operative Link on Gastritis Assessment (OLGA)Abstract
Introduction: Helicobacter pylori infection plays a critical role in the carcinogenesis cascade of intestinal gastric cancer. However, its prevalence in preneoplastic conditions generating changes in the gastric mucosa is unclear. Currently, endoscopic surveillance using the Sydney protocol is suggested every 2 to 3 years, but the presence of H. pylori infection in the subcardial region and gastric fundus is ill-defined.
Objective: to determine the prevalence and gastric location of H. pylori infection in patients with preneoplastic conditions.
Materials and methods: a cross-sectional study in adults with a previous diagnosis of atrophy or intestinal metaplasia who entered control endoscopy and were antrum, body, incisura angularis, subcardial region, and gastric fundus biopsied. A descriptive analysis of the results by gastric regions was performed.
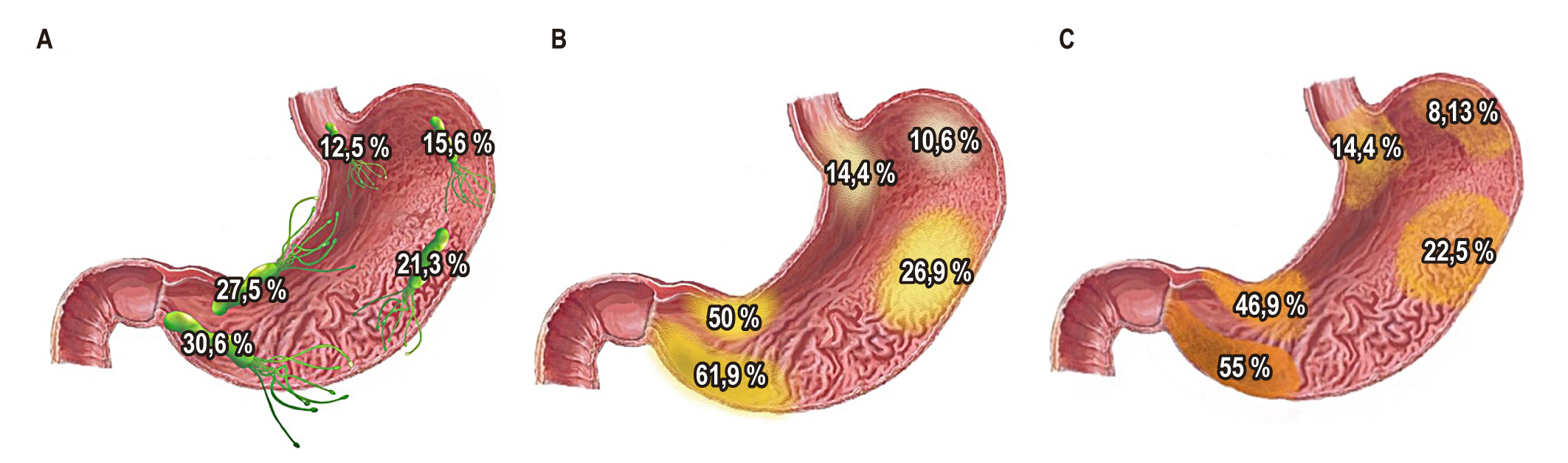
Results: data from 160 patients with a prevalence of H. pylori of 37.5% were collected. It increased from proximal to distal, starting with a 12.5% prevalence in the subcardial region to a 30.6% prevalence in the antrum. In addition, there was a similar pattern in the prevalence of preneoplastic lesions. Furthermore, advanced lesions (dysplasia, carcinoma) were observed in the incisura.
Conclusions: the prevalence of H. pylori in precancerous conditions showed a high presence in the distal regions compared to the proximal ones, and it is more frequent in the antrum and lower in the subcardial region. As for the gastric distribution of atrophy and metaplasia, more involvement was found in the antrum and angular notch and lower in the subcardial region and fundus.
Downloads
References
Otero Regino W, Gómez MA, Castro D. Gastric carcinogenesis. Rev Colomb Gastroenterol. 2009;24(3):314-329.
Van Cutsem E, Sagaert X, Topal B, Haustermans K, Prenen H. Gastric cancer. Lancet (London, England). 2016;388(10060):2654-2664. https://doi.org/10.1016/S0140-6736(16)30354-3
Cáncer en cifras [Internet]. Instituto Nacional de Cancerología; 2020 [consultado el 16 de febrero de 2021]. Disponible en: https://www.cancer.gov.co/medios-comunicacion-1/multimedia/destacados/cancer-cifras-1
Sgouras DN, Trang TTH, Yamaoka Y. Pathogenesis of Helicobacter pylori Infection. Helicobacter. 2015;20 Suppl 1(0 1):8-16. https://doi.org/10.1111/hel.12251
Correa P. Gastric cancer: an infectious disease. Rev Colomb Cirugía. 2011;26(2):111-117.
Dinis-Ribeiro M, Areia M, De Vries AC, Marcos-Pinto R, Monteiro-Soares M, O’Connor A, et al. Management of precancerous conditions and lesions in the stomach (MAPS): Guideline from the European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter Study Group (EHSG), European Society of Pathology (ESP), and the Sociedade Portuguesa. Virchows Arch. 2012;460(1):19-46. https://doi.org/10.1007/s00428-011-1177-8
Regino W. El gastroenterólogo y la gastritis crónica en la práctica clínica diaria. Rev Colomb Gastroenterol. 2010;25(3):301-305. www.scielo.unal.edu.co/scielo.php?script=sci_arttext&pid
Lee Y-C, Chiang T-H, Chou C-K, Tu YK, Liao WC, Wu MS, et al. Association Between Helicobacter pylori Eradication and Gastric Cancer Incidence: A Systematic Review and Meta-analysis. Gastroenterology. 2016;150(5):1113-1124.e5. https://doi.org/10.1053/j.gastro.2016.01.028
Lu C, Yu Y, Li L, Yu C, Xu P. Systematic review of the relationship of Helicobacter pylori infection with geographical latitude, average annual temperature and average daily sunshine. BMC Gastroenterol. 2018 Apr 17;18(1):50. https://doi.org/10.1186/s12876-018-0779-x
An international association between Helicobacter pylori infection and gastric cancer. The EUROGAST Study Group. Lancet (London, England). 1993;341(8857):1359-1362. https://doi.org/10.1016/0140-6736(93)90938-D
Correa P. Cáncer gástrico: una enfermedad infecciosa. Rev Colomb Cir. 2011;26:111-117.
Yoo JY, Kim N, Park YS, Hwang JH, Kim JW, Jeong SH, et al. Detection rate of Helicobacter pylori against a background of atrophic gastritis and/or intestinal metaplasia. J Clin Gastroenterol. 2007;41(8):751-755. https://doi.org/10.1097/MCG.0b013e31802c347d
Pimentel-Nunes P, Libânio D, Marcos-Pinto R, Areia M, Leja M, Esposito G, et al. Management of epithelial precancerous conditions and lesions in the stomach (MAPS II): European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter and Microbiota Study Group (EHMSG), European Society of Pathology (ESP), and Sociedade Portuguesa de Endoscopia Digestiva (SPED) guideline update 2019. Endoscopy. 2019;51(4):365-388. https://doi.org/10.1055/a-0859-1883
Tsukamoto T, Nakagawa M, Kiriyama Y, Toyoda T, Cao X. Prevention of Gastric Cancer: Eradication of Helicobacter Pylori and Beyond. Int J Mol Sci. 2017;18(8):1699. https://doi.org/10.3390/ijms18081699
Correa S, Cardona AF, Correa T, García HI, Estrada S. Prevalencia de Helicobacter pylori y características histopatológicas en biopsias gástricas de pacientes con síntomas dispépticos en un centro de referencia de Medellín. Rev Colomb Gastroenterol. 2016;31(1):9-15. https://doi.org/10.22516/25007440.67
Kim N, Park YS, Cho S Il, Lee HS, Choe G, Kim IW, et al. Prevalence and risk factors of atrophic gastritis and intestinal metaplasia in a korean population Without significant gastroduodenal disease. Helicobacter. 2008;13(4):245-255. https://doi.org/10.1111/j.1523-5378.2008.00604.x
Almouradi T, Hiatt T, Attar B. Gastric Intestinal Metaplasia in an Underserved Population in the USA: Prevalence, Epidemiologic and Clinical Features. Gastroenterol Res Pract. 2013;2013:856256. https://doi.org/10.1155/2013/856256
Kim HJ, Choi BY, Byun TJ, Eun CS, Song KS, Kim YS, et al. [The prevalence of atrophic gastritis and intestinal metaplasia according to gender, age and Helicobacter pylori infection in a rural population]. J Prev Med Public Health. 2008;41(6):373-379. https://doi.org/10.3961/jpmph.2008.41.6.373
Park YH, Kim N. Review of Atrophic Gastritis and Intestinal Metaplasia as a Premalignant Lesion of Gastric Cancer. J Cancer Prev. 2015;20(1):25-40. https://doi.org/10.15430/JCP.2015.20.1.25
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |















