Gastrointestinal food allergy: Prevalence, characterization, and direct costs in a referral center in Bogotá
DOI:
https://doi.org/10.22516/25007440.789Keywords:
Food hypersensitivity, Gastrointestinal, Characterization, Pediatrics, Prevalence, CostsAbstract
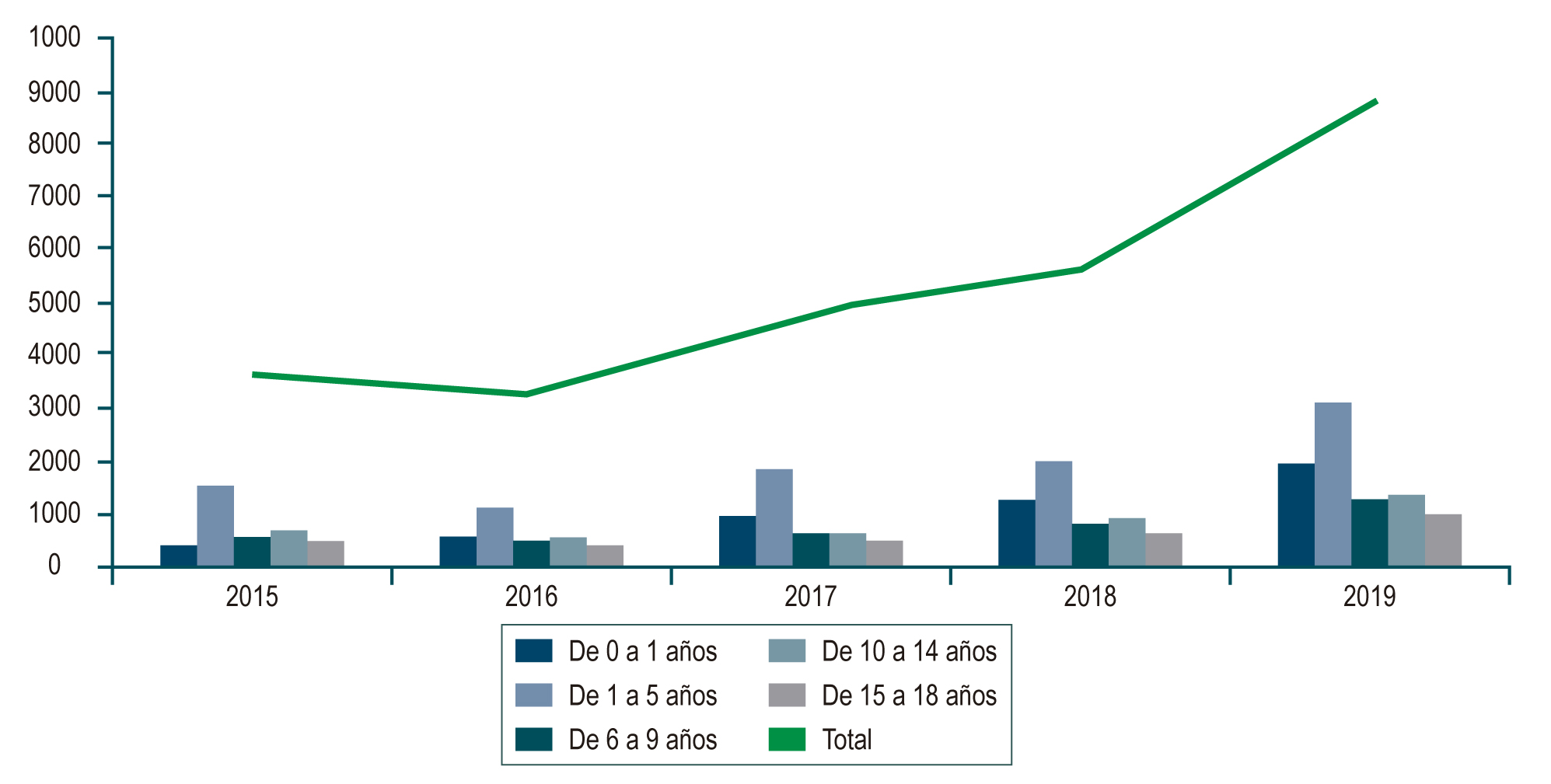
Introduction: The prevalence and incidence of gastrointestinal food allergy has increased in recent years with high associated costs, but usually with a good prognosis; nonetheless, in Colombia, information is scarce. This study intends to describe demographic variables, symptomatology, clinical picture, nutritional status, management, and natural history of the disease, determine its prevalence in the Colombian pediatric population by age group, and describe its direct costs.
Materials and methods: The study was conducted in three phases. In the first, we estimated the prevalence of the disease from the review of the RIPS and MIPRES databases between 2015 and 2019. Secondly, we checked the medical records selected per the inclusion and exclusion criteria for characterization and costs. Lastly, through a telephone survey, we asked about the current state of the disease and its resolution.
Results: The estimated prevalence adjusted for underreporting was 0.04 % for the pediatric population and 0.148 % for those under five. The most frequent diagnoses were allergic proctocolitis (59.3 %) and secondary functional gastrointestinal disorders (13.9 %). The most frequent allergen was cow’s milk protein. Early management is related to an excellent nutritional prognosis. Direct costs are mainly related to using formulas (92 %) and medical appointments (3.4 %); 89 % of parents consider that the food allergy will resolve over time.
Conclusions: This retrospective study is the most extensive in Colombia, drawing local conclusions that may be compared with other countries.
Downloads
References
Eiwegger T, Hung L, San Diego KE, O’Mahony L, Upton J. Recent developments and highlights in food allergy. Allergy. 2019;74(12):2355-2367. https://doi.org/10.1111/all.14082
Morita H, Nomura I, Matsuda A, Saito H, Matsumoto K. Gastrointestinal food allergy in infants. Allergol Int. 2013;62(3):297-307. https://doi.org/10.2332/allergolint.13-RA-0542
Bagés M, Chinchilla C, Ortiz C, Plata C, Puello E, Quintero O, et al. Recomendaciones sobre diagnóstico y tratamiento de la alergia a la proteína de la leche de vaca en población pediátrica colombiana. Posición de expertos. Rev Colomb Gastroenterol. 2020,35(1):54-64. https://doi.org/10.22516/25007440.405
Heine RG. Pathophysiology, diagnosis and treatment of food protein-induced gastrointestinal diseases. Curr Opin Allergy Clin Immunol. 2004;4(3):221-9. https://doi.org/10.1097/00130832-200406000-00015
Prescott SL, Pawankar R, Allen KJ, Campbell DE, Sinn JKh, Fiocchi A, et al. A global survey of changing patterns of food allergy burden in children. World Allergy Organ J. 2013;6(1):21. https://doi.org/10.1186/1939-4551-6-21
Lifschitz C, Szajewska H. Cow’s milk allergy: evidence-based diagnosis and management for the practitioner. Eur J Pediatr. 2015;174(2):141-50. https://doi.org/10.1007/s00431-014-2422-3
De Martinis M, Sirufo MM, Suppa M, Ginaldi L. New Perspectives in Food Allergy. Int J Mol Sci. 2020;21(4):1474. https://doi.org/10.3390/ijms21041474
van den Hoogen SC, van de Pol AC, Meijer Y, Toet J, van Klei C, de Wit NJ. Suspected cow’s milk allergy in everyday general practice: a retrospective cohort study on health care burden and guideline adherence. BMC Res Notes. 2014;7:507. https://doi.org/10.1186/1756-0500-7-507
Høst A, Halken S, Jacobsen HP, Christensen AE, Herskind AM, Plesner K. Clinical course of cow›s milk protein allergy/intolerance and atopic diseases in childhood. Pediatr Allergy Immunol. 2002;13(s15):23-8. https://doi.org/10.1034/j.1399-3038.13.s.15.7.x
Vanto T, Helppilä S, Juntunen-Backman K, Kalimo K, Klemola T, Korpela R, Koskinen P. Prediction of the development of tolerance to milk in children with cow›s milk hypersensitivity. J Pediatr. 2004;144(2):218-22. https://doi.org/10.1016/j.jpeds.2003.10.063
Patel DA, Holdford DA, Edwards E, Carroll NV. Estimating the economic burden of food-induced allergic reactions and anaphylaxis in the United States. J Allergy Clin Immunol. 2011;128(1):110-115.e5. https://doi.org/10.1016/j.jaci.2011.03.013
Vera JF, Ramirez A. Síntomas digestivos y respuesta clínica en lactantes con alergia a la proteína de leche de vaca. Rev Chil Pediatr. 2013;84(6):641-9. https://doi.org/10.4067/S0370-41062013000600007
Sistema de Información de Prestaciones de Salud - RIPS [Internet]. Bogotá: Ministerio de Salud y Protección Social; 2021 [acceso el 6 de febrero de 2021]. Disponible en: https://www.minsalud.gov.co/proteccionsocial/Paginas/rips.aspx
Morais MB, Spolidoro JV, Vieira MC, Cardoso AL, Clark O, Nishikawa A, et al. Amino acid formula as a new strategy for diagnosing cow’s milk allergy in infants: is it cost-effective? J Med Econ. 2016;19(12):1207-1214. https://doi.org/10.1080/13696998.2016.1211390
Instituto Nacional de Salud, Observatorio Nacional de Salud. Quinto informe ONS: Carga de enfermedad por enfermedades crónicas no transmisibles y discapacidad en Colombia. Bogotá D.C.: INS; 2015.
Grabenhenrich L, Trendelenburg V, Bellach J, Yürek S, Reich A, Fiandor A, et al. Frequency of food allergy in school-aged children in eight European countries-The EuroPrevall-iFAAM birth cohort. Allergy. 2020;75(9):2294-2308. https://doi.org/10.1111/all.14290
Gupta RS, Warren CM, Smith BM, Blumenstock JA, Jiang J, Davis MM, et al. The Public Health Impact of Parent-Reported Childhood Food Allergies in the United States. Pediatrics. 2018;142(6):e20181235. https://doi.org/10.1542/peds.2018-1235
Schoemaker AA, Sprikkelman AB, Grimshaw KE, Roberts G, Grabenhenrich L, Rosenfeld L, et al. Incidence and natural history of challenge-proven cow’s milk allergy in European children--EuroPrevall birth cohort. Allergy. 2015;70(8):963-72. https://doi.org/10.1111/all.12630
Koletzko S, Heine RG. Non-IgE mediated cow’s milk allergy in EuroPrevall. Allergy. 2015;70(12):1679-80. https://doi.org/10.1111/all.12681
Vieira MC, Morais MB, Spolidoro JV, Toporovski MS, Cardoso AL, Araujo GT, Nudelman V, Fonseca MC. A survey on clinical presentation and nutritional status of infants with suspected cow’ milk allergy. BMC Pediatr. 2010;10:25. https://doi.org/10.1186/1471-2431-10-25
Meyer R, Fleming C, Dominguez-Ortega G, Lindley K, Michaelis L, Thapar N, et al. Manifestations of food protein induced gastrointestinal allergies presenting to a single tertiary paediatric gastroenterology unit. World Allergy Organ J. 2013;6(1):13. https://doi.org/10.1186/1939-4551-6-13.
Sladkevicius E, Nagy E, Lack G, Guest JF. Resource implications and budget impact of managing cow milk allergy in the UK. J Med Econ. 2010;13(1):119-28. https://doi.org/10.3111/13696990903543242
Luyt D, Ball H, Makwana N, Green MR, Bravin K, Nasser SM, et al. BSACI guideline for the diagnosis and management of cow’s milk allergy. Clin Exp Allergy. 2014;44(5):642-72. https://doi.org/10.1111/cea.12302
Høst A, Husby S, Osterballe O. A prospective study of cow›s milk allergy in exclusively breast-fed infants. Incidence, pathogenetic role of early inadvertent exposure to cow›s milk formula, and characterization of bovine milk protein in human milk. Acta Paediatr Scand. 1988;77(5):663-70. https://doi.org/10.1111/j.1651-2227.1988.tb10727.x
Montijo-Barrios E, López-Ugalde MV, Ramírez-Mayans J, Anaya-Flórez MS, Arredondo-García JL, Azevedo-Tenorio I, et al. Guía latinoamericana para el diagnóstico y tratamiento de alergia a las proteínas de la leche de vaca (GL-APLV). Rev Invest Clin. 2014;66 Suppl 2:S9-S72.
Dierick BJH, van der Molen T, Flokstra-de Blok BMJ, Muraro A, Postma MJ, Kocks JWH, et al. Burden and socioeconomics of asthma, allergic rhinitis, atopic dermatitis and food allergy. Expert Rev Pharmacoecon Outcomes Res. 2020;20(5):437-453. https://doi.org/10.1080/14737167.2020.1819793
Papadopoulou A, Koletzko S, Heuschkel R, Dias JA, Allen KJ, Murch SH, et al. Management guidelines of eosinophilic esophagitis in childhood. J Pediatr Gastroenterol Nutr. 2014;58(1):107-18. https://doi.org/10.1097/MPG.0b013e3182a80be1
Saps M, Nichols-Vinueza DX, Rosen JM, Velasco-Benítez CA. Prevalence of functional gastrointestinal disorders in Colombian school children. J Pediatr. 2014;164(3):542-5.e1. https://doi.org/10.1016/j.jpeds.2013.10.088
Morita H, Nomura I, Matsuda A, Saito H, Matsumoto K. Gastrointestinal food allergy in infants. Allergol Int. 2013;62(3):297-307. https://doi.org/10.2332/allergolint.13-RA-0542
Sekerel BE, Seyhun O. Expert panel on practice patterns in the management of cow›s milk protein allergy and associated economic burden of disease on health service in Turkey. J Med Econ. 2017;20(9):923-930. https://doi.org/10.1080/13696998.2017.1342171
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














