Malacoplakia in a teenager: A case report
DOI:
https://doi.org/10.22516/25007440.475Keywords:
Malacoplakia, Gastrointestinal tract, ColonAbstract
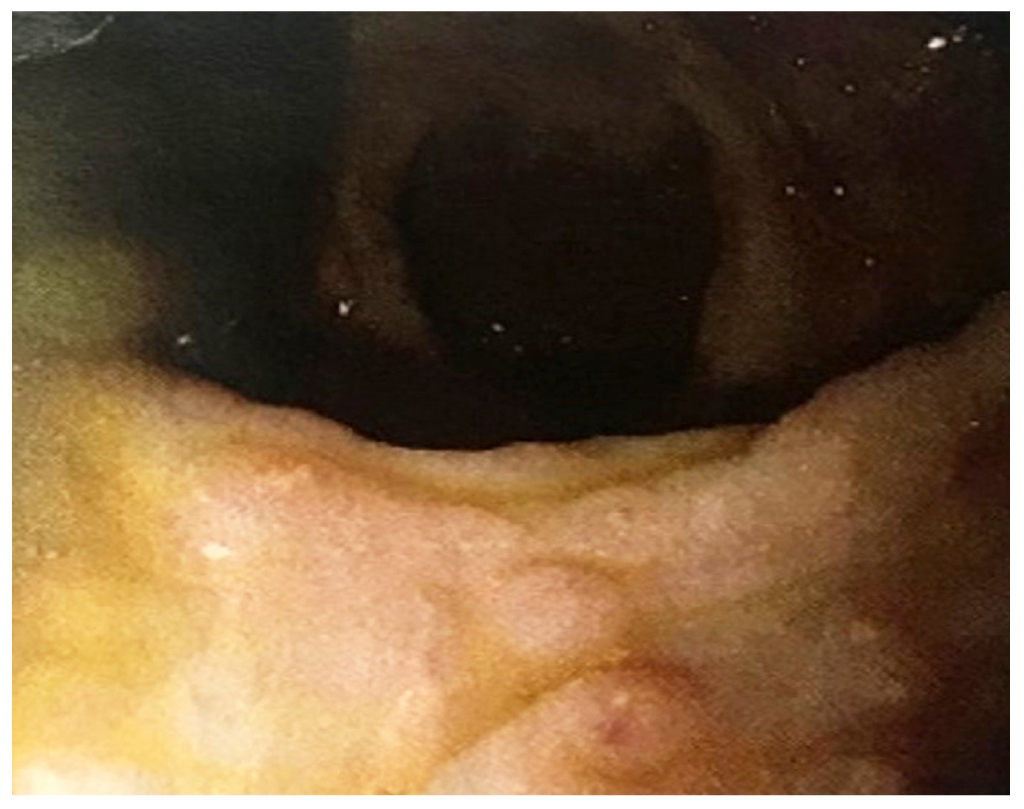
Malacoplakia is a rare, granulomatous, chronic inflammatory disease characterized by foamy histiocytic infiltrations known as Michaelis-Gutmann inclusions. The urinary system is the most commonly affected site, followed by the gastrointestinal tract. The prognosis of the disease depends on the extent, location, and underlying health status of the patient. This is the clinical case of a 15-year-old male patient with no significant health history. At age 7, the patient presented with hematochezia and mild abdominal pain that improved after defecation. A colonoscopy was performed, finding pseudopolypoid lesions in the sigmoid colon. Biopsy samples were taken, and the report showed inflammatory polyps with exacerbation foci, numerous histiocytes (Michaelis-Gutmann bodies), and reactive epithelial changes that lead to diagnose malacoplakia. Conclusion: Malacoplakia is a very rare disease in young people with no underlying disease. Its prevalence is unknown, but more than 700 cases have been reported. It can occur at all ages, with a mean age at diagnosis of 50 years. Pediatric cases are rare. There is a higher incidence in men, and it has no racial predilection. Between 60 % and 80 % of cases involve the urinary tract (bladder, kidneys, and urethra); 15 % involve the digestive tract (left colon, sigmoid colon, rectum, and stomach); and, to a lesser extent, other areas such as skin, lungs, and central nervous system may be affected. The prognosis of the disease is usually good. This is the case of a healthy 15-year-old male with no apparent associated disease that illustrates the rarity of this presentation and the need for a high level of clinical suspicion to diagnose the disease.
Downloads
References
Yared RA, Badran HA, Kamareddine MH, Ghosn Y, Bou Khalil R, El Ajamy K, Chouairy C, Farhat SG. Colonic Malakoplakia: A Rare Finding in a Healthy Male. Case Rep Gastroenterol. 2018;12(2):453-456. https://doi.org/10.1159/000492208
Yen JM, Soh NWY, Petersson F, Pandya G. Rectosigmoid malakoplakia. BMJ Case Rep. 017;2017:bcr2017219464.
https://doi.org/10.1136/bcr-2017-219464
Hyun KH, Shin HD, Kim DH. Malakoplakia in a healthy young female patient. Korean J Intern Med. 2013;28(4):475-80. https://doi.org/10.3904/kjim.2013.28.4.475
Matter MJ, Gygi C, Gillet M, Gebhard S, Bouzourene H. Malacoplakia simulating organ invasion in a rectosigmoid adenocarcinoma: report of a case. Dis Colon Rectum. 2001;44(9):1371-5. https://doi.org/10.1007/BF02234800
Biggar WD, Crawford L, Cardella C, Bear RA, Gladman D, Reynolds WJ. Malakoplakia and immunosuppressive therapy. Reversal of clinical and leukocyte abnormalities after withdrawal of prednisone and azathioprine. Am J Pathol. 1985;119(1):5-11.
Edmund L, Mohammed W. Colonic Carcinoma Associated with Malakoplakia. West Indian Med J. 2014;63(6):664-6. https://doi.org/10.7727/wimj.2014.079
Mitchell A, Dugas A. Malakoplakia of the colon following renal transplantation in a 73 year old woman: report of a case presenting as intestinal perforation. Diagn Pathol. 2019;14(1):22. https://doi.org/10.1186/s13000-019-0799-z
McClure J. Malakoplakia of the gastrointestinal tract. Postgrad Med J. 1981;57(664):95-103. https://doi.org/10.1136/pgmj.57.664.95
Guha S, Liu H. Malakoplakia of the Pancreas with Simultaneous Colon Involvement: Case Report and Review of the Literature. Case Rep Pathol. 2015;2015:649136. https://doi.org/10.1155/2015/649136
Karasavvidou F, Potamianos SP, Barbanis S, Stathakis E, Psychos A, Kapsoritakis AN, Koukoulis G. Malakoplakia of the colon associated with colonic adenocarcinoma diagnosed in colonic biopsies. World J Gastroenterol. 2007;13(45):6109-11. https://doi.org/10.3748/wjg.v13.45.6109
Lewin KJ, Fair WR, Steigbigel RT, Winberg CD, Droller MJ. Clinical and laboratory studies into the pathogenesis of malacoplakia. J Clin Pathol. 1976;29(4):354-363. https://doi.org/10.1136/jcp.29.4.354
Yousef GM, Naghibi B, Hamodat MM. Malakoplakia outside the urinary tract. Arch Pathol Lab Med. 2007;131(2):297-300. https://doi.org/10.1043/1543-2165(2007)131[297:MOTUT]2.0.CO;2
Alavian SM, Raissi Shabari F, Kamalian N. Malakoplakia of the colon: a case report and literature review, Med J Islamic Rep Iran. 2001;15(3):179-182.
Thorlacius H, Jerkeman A, Marginean FE, Toth E. Colorectal malakoplakia in a patient with hypogammaglobulinemia. Gastrointest Endosc. 2018;88(3):563-565. https://doi.org/10.1016/j.gie.2018.04.001
Asiyanbola B, Camuto P, Mansourian V. Malakoplakia occurring in association with colon carcinoma. J Gastrointest Surg. 2006;10(5):657-61. https://doi.org/10.1016/j.gassur.2005.09.015
Jadhav MN, Patil RK, Kittur SK, Yadav J. Colorectal malakoplakia in a child presenting as multiple polyposis coli. Indian J Pathol Microbiol. 2015;58(1):86-8. https://doi.org/10.4103/0377-4929.151197
van Furth R, van’t Wout JW, Wertheimer PA, Zwartendijk J. Ciprofloxacin for treatment of malakoplakia. Lancet. 1992;339(8786):148-9. https://doi.org/10.1016/0140-6736(92)90212-l
Fudaba H, Ooba H, Abe T, Kamida T, Wakabayashi Y, Nagatomi H, Fujiki M. An adult case of cerebral malakoplakia successfully cured by treatment with antibiotics, bethanechol and ascorbic acid. J Neurol Sci. 2014;342(1-2):192-6. https://doi.org/10.1016/j.jns.2014.05.006
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














