Immunoglobulin G4-Related Disease, A Diagnosis to Take into Account: About a Case
DOI:
https://doi.org/10.22516/25007440.978Keywords:
IgG4-Related Disease, autoimmune pancreatitis, Immunoglobulin G4Abstract
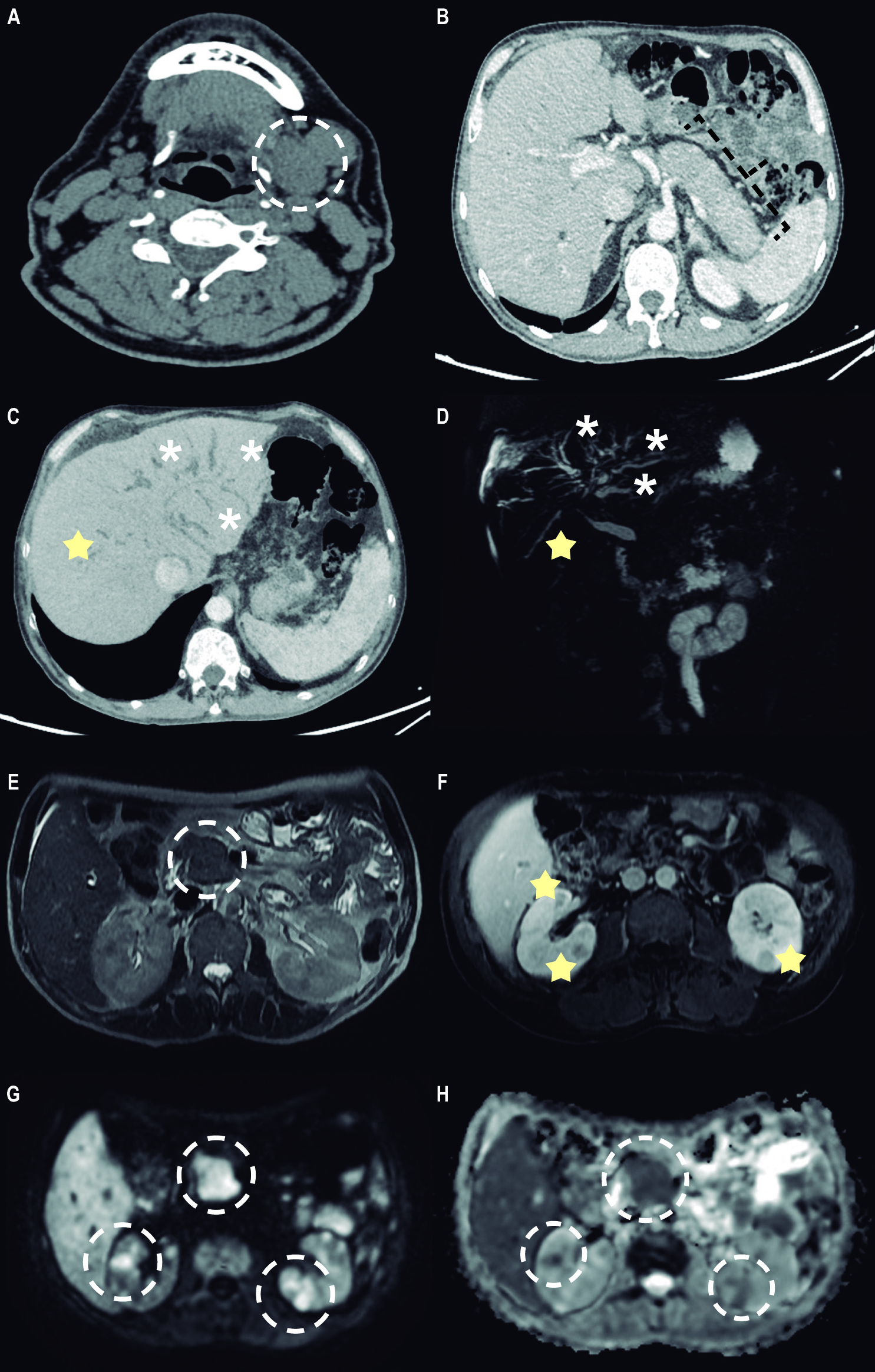
Immunoglobulin G4-related disease (IgG4-RD) is an immune-mediated and multisystemic condition associated with developing fibroinflammatory lesions in any organ. The diagnosis is made based on the sum of clinical, serological, radiological, and histopathological criteria; however, this is often difficult due to its similarity to neoplasms, infections, or other immune-mediated diseases. Treatment is based on corticosteroids, in a possible combination with immunomodulators. The present case concerns a 59-year-old man with a history of jaundice syndrome and weight loss, admitted for suspected malignant neoplasia of the bile duct. Imaging revealed stricture with dilation of the intrahepatic bile ducts, prominent pancreas, pancreatic duct stricture, and nodular renal lesions. Due to the history of left submandibulectomy two years before the current disease and histology compatible with Küttner’s tumor, plus the high IgG4 serum values, the diagnosis of IgG4-RD was established. He started treatment with corticosteroids and was asymptomatic during follow-up.
Downloads
References
Stone JH, Zen Y, Deshpande V. Mechanisms of disease: IgG4-related disease. N Engl J Med. 2012;366(6):539-51. https://doi.org/10.1056/NEJMRA1104650
Ruiz-Rebollo ML, Álvarez-Quiñones-Sanz M, Fuertes-Alija JJ, Izquierdo-Santervás S. IgG4-related disease mimicking pancreatic tumour. Gastroenterología y Hepatología (English Edition). 2021;44(9):660–1. https://doi.org/10.1016/J.GASTRE.2020.07.026
Kamisawa T, Zen Y, Pillai S, Stone JH. IgG4-related disease. Lancet. 2015;385(9976):1460–71. https://doi.org/10.1016/S0140-6736(14)60720-0
Johnston J, Allen JE. IgG4-related disease in the head and neck. Curr Opin Otolaryngol Head Neck Surg. 2018;26(6):403–8. https://doi.org/10.1097/MOO.0000000000000487
Skillington SA, Ogden MA. IgG4-Related Disease and the Salivary Glands: A Review of Pathophysiology, Diagnosis, and Management. Otolaryngol Clin North Am. 2021;54(3):497–508. https://doi.org/10.1016/J.OTC.2021.02.002
Wallace ZS, Perugino C, Matza M, Deshpande V, Sharma A, Stone JH. IgG4-Related Disease. Clin Chest Med. 2019;40(3):583-97. https://doi.org/10.1016/J.CCM.2019.05.005
Wallace ZS, Naden RP, Chari S, Choi H, Della-Torre E, Dicaire JF, et al. The 2019 American College of Rheumatology/European League Against Rheumatism Classification Criteria for IgG4-Related Disease. Arthritis Rheumatol. 2020;72(1):7–19. https://doi.org/10.1002/ART.41120
Khosroshahi A, Wallace ZS, Crowe JL, Akamizu T, Azumi A, Carruthers MN, et al. International consensus guidance statement on the management and treatment of IgG4-related disease. Arthritis Rheumatol. 2015;67(7):1688–99. https://doi.org/10.1002/ART.39132
Yamamoto M, Yajima H, Takahashi H, Yokoyama Y, Ishigami K, Shimizu Y, et al. Everyday clinical practice in IgG4-related dacryoadenitis and/or sialadenitis: Results from the SMART database. Mod Rheumatol. 2015;25(2):199–204. https://doi.org/10.3109/14397595.2014.950036
Khosroshahi A, Carruthers MN, Deshpande V, Unizony S, Bloch DB, Stone JH. Rituximab for the treatment of IgG4-related disease: Lessons from 10 consecutive patients. Medicine. 2012;91(1):57–66. https://doi.org/10.1097/MD.0B013E3182431EF6
Carruthers MN, Topazian MD, Khosroshahi A, Witzig TE, Wallace ZS, Hart PA, et al. Rituximab for IgG4-related disease: a prospective, open-label trial. Ann Rheum Dis. 2015;74(6):1171–7. https://doi.org/10.1136/ANNRHEUMDIS-2014-206605
Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003;38(10):982-4. https://doi.org/10.1007/S00535-003-1175-Y
Uchida K, Masamune A, Shimosegawa T, Okazaki K. Prevalence of IgG4-Related Disease in Japan Based on Nationwide Survey in 2009. Int J Rheumatol. 2012;2012:358371. https://doi.org/10.1155/2012/358371
Masamune A, Kikuta K, Hamada S, Tsuji I, Takeyama Y, Shimosegawa T, et al. Nationwide epidemiological survey of autoimmune pancreatitis in Japan in 2016. J Gastroenterol. 2020;55(4):462-70. https://doi.org/10.1007/S00535-019-01658-7
Wallace ZS, Zhang Y, Perugino CA, Naden R, Choi HK, Stone JH. Clinical phenotypes of IgG4-related disease: an analysis of two international cross-sectional cohorts. Ann Rheum Dis. 2019;78(3):406–12. https://doi.org/10.1136/ANNRHEUMDIS-2018-214603
Zen Y, Nakanuma Y. IgG4-related disease: A cross-sectional study of 114 cases. Am J Surg Pathol, 2010;34(12):1812–9. https://doi.org/10.1097/PAS.0B013E3181F7266B
Pillai S, Perugino C, Kaneko N. Immune mechanisms of fibrosis and inflammation in IgG4-related disease. Curr Opin Rheumatol. 2020;32(2):146–51. https://doi.org/10.1097/BOR.0000000000000686
Della-Torre E, Feeney E, Deshpande V, Mattoo H, Mahajan V, Kulikova M, et al. B-cell depletion attenuates serological biomarkers of fibrosis and myofibroblast activation in IgG4-related disease. Ann Rheum Dis. 2015;74(12):2236. https://doi.org/10.1136/ANNRHEUMDIS-2014-205799
Chen Y, Lin W, Yang H, Wang M, Zhang P, Feng R, et al. Aberrant Expansion and Function of Follicular Helper T Cell Subsets in IgG4-Related Disease. Arthritis Rheumatol. 2018;70(11):1853–65. https://doi.org/10.1002/ART.40556
Furukawa S, Moriyama M, Tanaka A, Maehara T, Tsuboi H, Iizuka M, et al. Preferential M2 macrophages contribute to fibrosis in IgG4-related dacryoadenitis and sialoadenitis, so-called Mikulicz’s disease. Clinical Immunology. 2015;156(1):9–18. https://doi.org/10.1016/J.CLIM.2014.10.008
Lanzillotta M, Lanzillotta M, Mancuso G, Mancuso G, Della-Torre E. Advances in the diagnosis and management of IgG4 related disease. BMJ. 2020;369:m1067. https://doi.org/10.1136/BMJ.M1067
Bhatti RM, Stelow EB. IgG4-related disease of the head and neck. Adv Anat Pathol. 2013;20(1):10–6. https://doi.org/10.1097/PAP.0B013E31827B619E
Mulholland GB, Jeffery CC, Satija P, Côté DWJ. Immunoglobulin G4-related diseases in the head and neck: a systematic review. J Otolaryngol Head Neck Surg.2015;44(1):24. https://doi.org/10.1186/S40463-015-0071-9
Chari ST, Kloeppel G, Zhang L, Notohara K, Lerch MM, Shimosegawa T. Histopathologic and clinical subtypes of autoimmune pancreatitis: The honolulu consensus document. Pancreas. 2010;39(5):549–54. https://doi.org/10.1097/MPA.0B013E3181E4D9E5
Sah RP, Chari ST, Pannala R, Sugumar A, Clain JE, Levy MJ, et al. Differences in Clinical Profile and Relapse Rate of Type 1 Versus Type 2 Autoimmune Pancreatitis. Gastroenterology. 2010;139(1):140–8. https://doi.org/10.1053/J.GASTRO.2010.03.054
Vashi B, Khosroshahi A. IgG4-Related Disease with Emphasis on Its Gastrointestinal Manifestation. Gastroenterol Clin North Am. 2019;48(2):291–305. https://doi.org/10.1016/j.gtc.2019.02.008
Zheng Y, Elsayes KM, Waranch C, Abdelaziz A, Menias CO, Sandrasegaran K, et al. IgG4-related disease in the abdomen and pelvis: atypical findings, pitfalls, and mimics. Abdominal Radiology. 2020;45(8):2485–99. https://doi.org/10.1007/S00261-020-02526-2
Erkelens GW, Vleggaar FP, Lesterhuis W, van Buuren HR, van der Werf SDJ. Sclerosing pancreato-cholangitis responsive to steroid therapy. Lancet. 1999;354(9172):43–4. https://doi.org/10.1016/S0140-6736(99)00603-0
Smal AJ, Loftus CG, Smyrk TC, Baron TH. A case of IgG4-associated cholangitis and autoimmune pancreatitis responsive to corticosteroids. Nat Clin Pract Gastroenterol Hepatol. 2008(12):707–12. https://doi.org/10.1038/NCPGASTHEP1296
Nakazawa T, Ando T, Hayashi K, Naitoh I, Ohara H, Joh T. Diagnostic procedures for IgG4-related sclerosing cholangitis. J Hepatobiliary Pancreat Sci. 2011;18(2):127–36. https://doi.org/10.1007/S00534-010-0320-2
Mendes FD, Jorgensen R, Keach J, Katzmann JA, Smyrk T, Donlinger J, et al. Elevated serum IgG4 concentration in patients with primary sclerosing cholangitis. Am J Gastroenterol. 2006;101(9):2070–5. https://doi.org/10.1111/J.1572-0241.2006.00772.X
Itoi T, Kamisawa T, Igarashi Y, Kawakami H, Yasuda I, Itokawa F, et al. The role of peroral video cholangioscopy in patients with IgG4-related sclerosing cholangitis. Journal of Gastroenterology. 2012;48(4):504–14. https://doi.org/10.1007/S00535-012-0652-6
Saeki T, Ito T, Yamazaki H, Imai N, Nishi S. Hypocomplementemia of unknown etiology: an opportunity to find cases of IgG4-positive multi-organ lymphoproliferative syndrome. Rheumatology International. 2009;30(1):99–103. https://doi.org/10.1007/S00296-009-0925-4
Saeki T, Kawano M, Mizushima I, Yamamoto M, Wada Y, Nakashima H, et al. The clinical course of patients with IgG4-related kidney disease. Kidney Int. 2013;84(4):826–33. https://doi.org/10.1038/KI.2013.191
Carruthers MN, Khosroshahi A, Augustin T, Deshpande V, Stone JH. The diagnostic utility of serum IgG4 concentrations in IgG4-related disease. Ann Rheum Dis. 2015;74(1):14–8. https://doi.org/10.1136/ANNRHEUMDIS-2013-204907
Zhang W, Stone JH. Management of IgG4-related disease. Lancet Rheumatol. 2019;1(1):e55–65. https://doi.org/10.1016/S2665-9913(19)30017-7
Lanzillotta M, Fernàndez-Codina A, Culver E, Ebbo M, Martinez-Valle F, Schleinitz N, et al. Emerging therapy options for IgG4-related disease. Emerging therapy options for IgG4-related disease. Expert Rev Clin Immunol. 2021;17(5):471-83. https://doi.org/10.1080/1744666X.2021.1902310
Okazaki K, Chari ST, Frulloni L, Lerch MM, Kamisawa T, Kawa S, et al. International consensus for the treatment of autoimmune pancreatitis. Pancreatology. 2017;17(1):1–6. https://doi.org/10.1016/J.PAN.2016.12.003
Hart PA, Kamisawa T, Brugge WR, Chung JB, Culver EL, Czakó L, et al. Original article: Long-term outcomes of autoimmune pancreatitis: a multicentre, international analysis. Gut. 2013;62(12):1771. https://doi.org/10.1136/GUTJNL-2012-303617
Omar D, Chen Y, Cong Y, Dong L. Glucocorticoids and steroid sparing medications monotherapies or in combination for IgG4-RD: a systematic review and network meta-analysis. Rheumatology (Oxford). 2020;59(4):718–26. https://doi.org/10.1093/RHEUMATOLOGY/KEZ380
Deshpande V, Zen Y, Chan JKC, Yi EE, Sato Y, Yoshino T, et al. Consensus statement on the pathology of IgG4-related disease. Modern Pathology. 2012;25(9):1181–92. https://doi.org/10.1038/modpathol.2012.72
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














