Periampullary Mass as an Unusual Manifestation of Coccidioidomycosis. Case Report and Literature Review
DOI:
https://doi.org/10.22516/25007440.965Keywords:
Coccidioides, Colombia, Disseminated mycosis, icteric syndrome, Systemic mycosis, Periampullary neoplasmAbstract
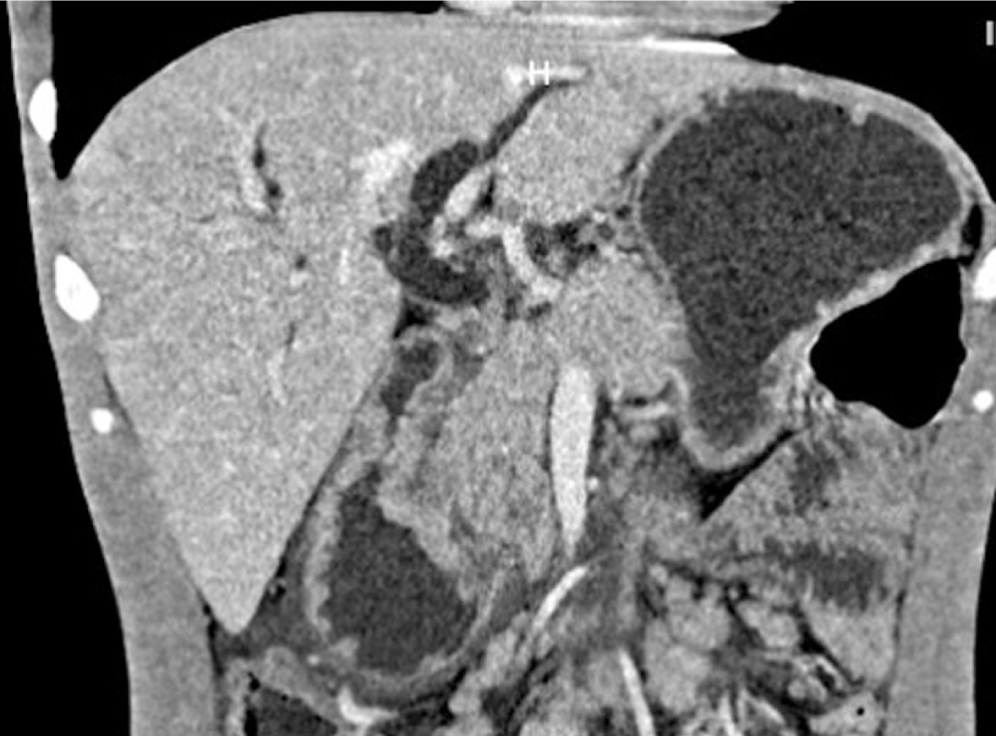
In Colombia, coccidioidomycosis is a rare entity, and the intestinal manifestation is infrequent, with around a dozen cases reported in the world literature. This article reports the case of a 29-year-old male Venezuelan immigrant with a 4-month history of abdominal pain, jaundice, nausea, and vomiting. The tomography and the endoscopic study revealed a circumferential exophytic mass in the second portion of the duodenum. The biopsy revealed multiple spherules filled with round fungal endospores with a final diagnosis of disseminated coccidioidomycosis. The patient was discharged before the final pathology report with fluconazole doses of 200 mg every other day and an order for outpatient magnetic resonance cholangiography for outpatient follow-up, which he has not attended.
Downloads
References
Coffin A, Boulay-Coletta I, Sebbag-Sfez D, Zins M. Radioanatomy of the retroperitoneal space. Diagn Interv Imaging. 2015;96(2):171-86. https://doi.org/10.1016/j.diii.2014.06.015
Barat M, Dohan A, Dautry R, Barral M, Boudiaf M, Hoeffel C, et al. Mass-forming lesions of the duodenum: A pictorial review. Diagn Interv Imaging. 2017;98(10):663-675. https://doi.org/10.1016/j.diii.2017.01.004
Ajello L. Comparative ecology of respiratory mycotic disease agents. Bacteriol Rev. 1967;31(1):6-24. https://doi.org/10.1128/br.31.1.6-24.1967
Laniado-Laborín R, Arathoon EG, Canteros C, Muñiz-Salazar R, Rendon A. Coccidioidomycosis in Latin America. Med Mycol. 2019;57(Supplement_1):S46-S55. https://doi.org/10.1093/mmy/myy037
Tintelnot K, De Hoog GS, Antweiler E, Losert H, Seibold M, Brandt MA, Van Den Ende AH, Fisher MC. Taxonomic and diagnostic markers for identification of Coccidioides immitis and Coccidioides posadasii. Med Mycol. 2007;45(5):385-93. https://doi.org/10.1080/13693780701288070
Forsbach Sánchez G, Fuentes Pensamiento R. Coccidioidomicosis pulmonar crónica progresiva en una paciente con diabetes mellitus tipo II. Rev Invest Clin. 1985;37(1):49-51.
Saubolle MA, McKellar PP, Sussland D. Epidemiologic, clinical, and diagnostic aspects of coccidioidomycosis. J Clin Microbiol. 2007;45(1):26-30. https://doi.org/10.1128/JCM.02230-06
Sales E. Coccidioidomicosis. Rev Médico-Quirúrgica Atlántico. 1958;2:289-94.
Robledo M. Coccidioidomycosis. Antioquia Med. 1965;15(5):361-2.
Canteros CE, Vélez HA, Toranzo AI, Suárez-Alvarez R, Tobón OÁ, Jimenez AMP, et al. Molecular identification of Coccidioides immitis in formalin-fixed, paraffin-embedded (FFPE) tissues from a Colombian patient. Med Mycol. 2015;53(5):520-7. https://doi.org/10.1093/mmy/myv019
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46(12):1813-21. https://doi.org/10.1086/588660
Odio CD, Marciano BE, Galgiani JN, Holland SM. Risk Factors for Disseminated Coccidioidomycosis, United States. Emerg Infect Dis. 2017;23(2):308–11. https://doi.org/10.3201/eid2302.160505
Bays DJ, Thompson GR 3rd. Coccidioidomycosis. Infect Dis Clin North Am. 2021;35(2):453-469. https://doi.org/10.1016/j.idc.2021.03.010
Galgiani JN, Ampel NM, Blair JE, Catanzaro A, Johnson RH, Stevens DA, et al. Coccidioidomycosis. Clin Infect Dis. 2005;41(9):1217-23. https://doi.org/10.1086/496991
Malik U, Cheema H, Kandikatla R, Ahmed Y, Chakrala K. Disseminated Coccidioidomycosis Presenting as Carcinomatosis Peritonei and Intestinal Coccidioidomycosis in a Patient with HIV. Case Rep Gastroenterol. 2017;11(1):114-9. https://doi.org/10.1159/000456655
Luna-Isaac JA, Muñiz-Salazar R, Baptista-Rosas RC, Enríquez-Paredes LM, Castañón-Olivares LR, Contreras-Pérez C, et al. Genetic analysis of the endemic fungal pathogens Coccidioides posadasii and Coccidioides immitis in Mexico. Med Mycol. 2014;52(2):156-66. https://doi.org/10.1093/mmy/myt005
Canteros CE, Toranzo A, Suárez-Alvarez R, Davel G, Castañon-Olivares LR, Nápoli J. Identidad genética del hongo causante del primer caso de coccidioidomicosis descripto por Alejandro Posadas en 1892. Medicina (B Aires). 2009;69(2):215-20.
Ampel NM, Robey I, Nguyen CT. An Analysis of Skin Test Responses to Spherulin-Based Coccidioidin (Spherusol®) Among a Group of Subjects with Various Forms of Active Coccidioidomycosis. Mycopathologia. 2019;184(4):533-538. https://doi.org/10.1007/s11046-019-00356-5
McHardy IH, Dinh BN, Waldman S, Stewart E, Bays D, Pappagianis D, et al. Coccidioidomycosis Complement Fixation Titer Trends in the Age of Antifungals. J Clin Microbiol. 2018;56(12):e01318-18. https://doi.org/10.1128/JCM.01318-18
Johnson RH, Einstein HE. Coccidioidal meningitis. Clin Infect Dis. 2006;42(1):103-7. https://doi.org/10.1086/497596
Galgiani JN, Catanzaro A, Cloud GA, Higgs J, Friedman BA, Larsen RA, et al. Fluconazole therapy for coccidioidal meningitis. The NIAID-Mycoses Study Group. Ann Intern Med. 1993;119(1):28-35. https://doi.org/10.7326/0003-4819-119-1-199307010-00005
Dewsnup DH, Galgiani JN, Graybill JR, Diaz M, Rendon A, Cloud GA, et al. Is it ever safe to stop azole therapy for Coccidioides immitis meningitis? Ann Intern Med. 1996;124(3):305-10. https://doi.org/10.7326/0003-4819-124-3-199602010-00004
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














