Compromiso gastrointestinal y hepático en Síndrome de Sjögren primario: reporte de caso y revisión de la literatura
DOI:
https://doi.org/10.22516/25007440.918Keywords:
Sjögren’s syndrome, Sclerosing cholangitis, Digestive system abnormalities, Antinuclear antibodies, Gastrointestinal diseasesAbstract
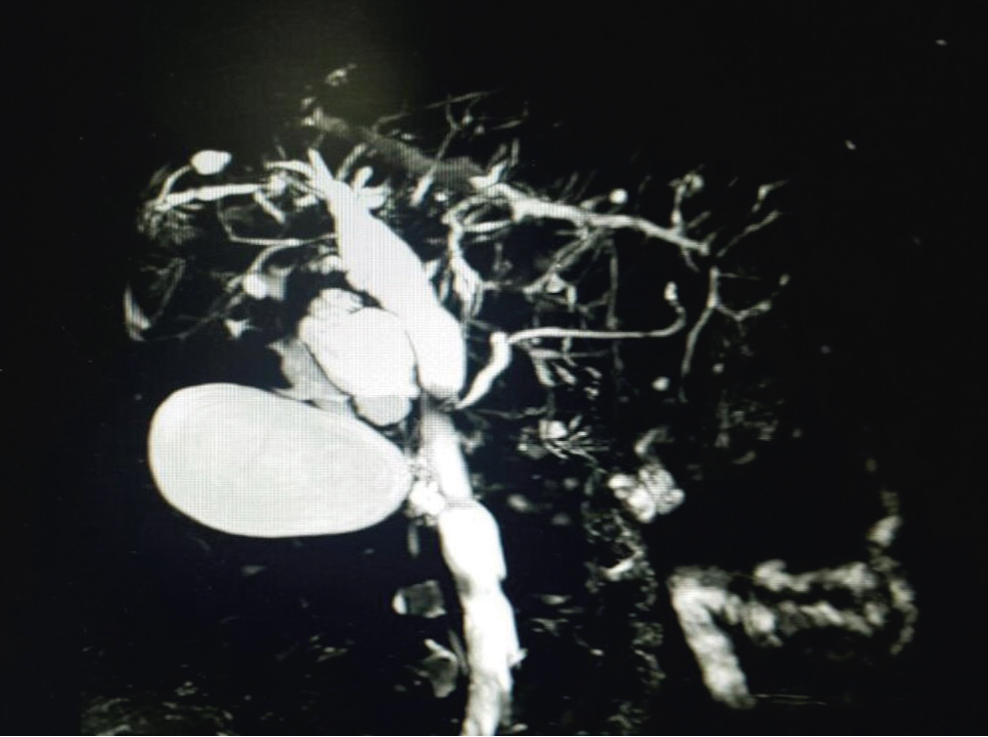
Sjögren's syndrome is a systemic autoimmune disease characterized by ocular and oral dryness due to exocrine gland involvement, however, it can manifest with gastrointestinal symptoms covering a wide spectrum ranging from esophageal and intestinal dysmotility, achalasia, hypochlorhydria, chronic atrophic gastritis, to pancreatic enzymodeficiency, biliary dysfunction and liver cirrhosis, presenting variation in its clinical manifestations, and associating erroneous approaches in many occasions. This article reviews the gastrointestinal manifestations of Sjögren's syndrome, and presents the case of a woman in the eighth decade of life with Sjögren's syndrome, presenting asymptomatic at hepatobiliary level, documentation of alteration in liver profile tests, and subsequent diagnosis of primary sclerosing cholangitis, receiving initial management with ursodeoxycholic acid and retrograde cholangiopancreatography with endoscopic dilatations. This association is infrequent and warrants special consideration.
Downloads
References
Ramos-Casals M, Brito-Zerón P, Sisó-Almirall A, Bosch X. Primary Sjögren syndrome. BMJ. 2012;345(7872):22700787. https://doi.org/10.1136/bmj.e3821
Vivino FB. Sjogren's syndrome: Clinical aspects. Clin Immunol. 2017;182:48-54. https://doi.org/10.1016/j.clim.2017.04.005
Tincani A, Andreoli L, Cavazzana I, Doria A, Favero M, Fenini MG, et al. Novel aspects of Sjögren's syndrome in 2012. BMC Med. 2013;11(1):1-2. https://doi.org/10.1186/1741-7015-11-93
Negrini S, Emmi G, Greco M, Borro M, Sardanelli F, Murdaca G, et al. Sjögren's syndrome: a systemic autoimmune disease. Clin Exp Med. 2022;22(1):9-25. https://doi.org/10.1007/s10238-021-00728-6
Ebert EC. Gastrointestinal and hepatic manifestations of Sjogren syndrome. J Clin Gastroenterol. 2012;46(1):25-30. https://doi.org/10.1097/MCG.0b013e3182329d9c
Zeron PB, Retamozo S, Bové A, Kostov BA, Sisó A, Ramos-Casals M. Diagnosis of liver involvement in primary sjögren syndrome. J Clin Transl Hepatol. 2013;1(2):94-102.
Ramos-Casals M, Sánchez-Tapias JM, Parés A, Forns X, Brito-Zerón P, Nardi N, et al. Characterization and differentiation of autoimmune versus viral liver involvement in patients with Sjögren's syndrome. J Rheumatol. 2006;33(8):1593-9.
Shi J, Li Z, Zeng X, Lin Y, Xie WF. Ursodeoxycholic acid in primary sclerosing cholangitis: Meta-analysis of randomized controlled trials. Hepatol Res. 2009;39(9):865-73. https://doi.org/10.1111/j.1872-034X.2009.00527.x
Poropat G, Giljaca V, Stimac D, Gluud C. Bile acids for primary sclerosing cholangitis. Cochrane Database Syst Rev. 2011;1-2. https://doi.org/10.1002/14651858.CD003626.pub2
Reksten TR, Jonsson M V. Sjögren's Syndrome: An update on epidemiology and current insights on pathophysiology. Oral Maxillofac Surg Clin North Am. 2014;26(1):1-12. https://doi.org/10.1016/j.coms.2013.09.002
Dawson LJ, Allison HE, Stanbury J, Fitzgerald D, Smith PM. Putative anti-muscarinic antibodies cannot be detected in patients with primary Sjögren's syndrome using conventional immunological approaches. Rheumatology. 2004;43(12):1488-95. https://doi.org/10.1093/rheumatology/keh389
Papas AS, Sherrer YS, Charney M, Golden HE, Medsger TA, Walsh BT, et al. Successful treatment of dry mouth and dry eye symptoms in Sjögren's syndrome patients with oral pilocarpine: A randomized, placebo-controlled, dose-adjustment study. J Clin Rheumatol. 2004;10(4):169-77. https://doi.org/10.1097/01.rhu.0000135553.08057.21
Mandl T, Ekberg O, Wollmer P, Manthorpe R, Jacobsson LTH. Dysphagia and dysmotility of the pharynx and oesophagus in patients with primary Sjögren's syndrome. Scand J Rheumatol. 2007;36(5):394-401. https://doi.org/10.1080/03009740701607638
Leone MC, Alunno A, Cafaro G, Valentini V, Marcucci E, Bartoloni E, et al. The clinical spectrum of primary sjögren's syndrome: Beyond exocrine glands. Reumatismo. 2017;69(3):93-100. https://doi.org/10.4081/reumatismo.2017.1032
Waterman SA, Gordon TP, Rischmueller M. Inhibitory effects of muscarinic receptor autoantibodies on parasympathetic neurotransmission in Sjogren's syndrome. Arthritis Rheum. 2000;43(7):1647-54. https://doi.org/10.1002/1529-0131(200007)43:7<1647::AID-ANR31>3.0.CO;2-P
Kjellén G, Fransson SG, Lindström F, Sökjer H, Tibbling L. Esophageal function, radiography, and dysphagia in Sjögren's syndrome. Dig Dis Sci. 1986;31(3):225-9. https://doi.org/10.1007/BF01318111
Grande L, Lacima G, Ros E, Font J, Pera C. Esophageal Motor Function in Primary Sjögren's Syndrome. Am J Gastroenterol. 1993;88(3):378-81.
Türk T, Pirildar T, Tunç E, Bor S, Doğanavşargil E. Manometric assessment of esophageal motility in patients with primary Sjögren's syndrome. Rheumatol Int. 2005;25(4):246-9. https://doi.org/10.1007/s00296-003-0426-9
Rosztóczy A, Kovács L, Wittmann T, Lonovics J, Pokorny G. Manometric assessment of impaired esophageal motor function in primary Sjögren's syndrome. Clin Exp Rheumatol. 2001;19(2):147-52.
Parra-Izquierdo V, Bernal Macías S, Avila F et al. Parra-Izquierdo V, Bernal Macías S, Avila F, et al. In: Serie de casos de pacientes con enfermedad de tejido conectivo no esclerodermia con alteraciones motoras esofagicas y anorectales por manometria de alta resolución en el Hospital Universitario San Ignacio durante el 2016. Bucaramanga, Colombia.; 2017.
Belafsky PC, Postma GN. The laryngeal and esophageal manifestations of Sjögren's syndrome. Curr Rheumatol Rep. 2003;5(4):297-303. https://doi.org/10.1007/s11926-003-0008-6
El Miedany YM, Baddour M, Ahmed I, Fahmy H. Sjogren's syndrome: Concomitant H. Pylori infection and possible correlation with clinical parameters. Jt Bone Spine. 2005;72(2):135-41. https://doi.org/10.1016/j.jbspin.2004.04.005
Buchanan WW, Cox AG, Harden RM, Glen AI, Anderson JR, Gray KG. Gastric studies in sjögren's syndrome. Gut. 1966;7(4):351-4. https://doi.org/10.1136/gut.7.4.351
Kilpi A, Bergroth V, Konttinen YT, Maury CPJ, Reitamo S, Wegelius O. Lymphocyte infiltrations of the gastric mucosa in sjöugren's syndrome. An Immunoperoxidase Study Using Monoclonal Antibodies in the Avidin‐Biotin‐Peroxidase Method. Arthritis Rheum. 1983;26(10):1196-200. https://doi.org/10.1002/art.1780261004
Maury CPJ, Törnroth T, Teppo A ‐M. Atrophic gastritis in sjögren's syndrome. Morphologic, biochemical, and immunologic findings. Arthritis Rheum. 1985;28(4):388-94. https://doi.org/10.1002/art.1780280406
Brito-Zerón P, Kostov B, Fraile G, Caravia-Durán D, Maure B, Rascón FJ, et al. Characterization and risk estimate of cancer in patients with primary Sjögren syndrome. J Hematol Oncol. 2017;10(1):17-8. https://doi.org/10.1186/s13045-017-0464-5
Kim-Lee C, Suresh L, Ambrus JL. Gastrointestinal disease in Sjogren's syndrome: related to food hypersensitivities. Springerplus. 2015;4(1):1-5. https://doi.org/10.1186/s40064-015-1557-7
Iltanen S, Collin P, Korpela M, Holm K, Partanen J, Polvi A, et al. Celiac Disease and Markers of Celiac Disease Latency in Patients With Primary Sjögren's Syndrome. Am J Gastroenterol. 1999;94(4):1042-6. https://doi.org/10.1111/j.1572-0241.1999.01011.x
https://doi.org/10.1016/S0002-9270(99)00066-0
Szodoray P, Barta Z, Lakos G, Szakáll S, Zeher M. Coeliac disease in Sjögren's syndrome - A study of 111 Hungarian patients. Rheumatol Int. 2004;24(5):278-82. https://doi.org/10.1007/s00296-003-0360-x
Doyle MK. Vasculitis associated with connective tissue disorders. Curr Rheumatol Rep. 2006;8(4):312-6. https://doi.org/10.1007/s11926-006-0015-5
Palm Ø, Moum B, Gran JT. Estimation of Sjögren's syndrome among IBD patients: A six year post-diagnostic prevalence study. Scand J Rheumatol. 2002;31(3):140-5. https://doi.org/10.1080/rhe.31.3.140.145
De Paiva CS, Jones DB, Stern ME, Bian F, Moore QL, Corbiere S, et al. Altered Mucosal Microbiome Diversity and Disease Severity in Sjögren Syndrome. Sci Rep. 2016;6:18-9. https://doi.org/10.1038/srep23561
Barton A, Pal B, Whorwell PJ, Marshall D. Increased prevalence of sicca complex and fibromyalgia in patients with irritable bowel syndrome. Am J Gastroenterol. 1999;94(7):1898-901. https://doi.org/10.1111/j.1572-0241.1999.01146.x
Mandl T, Marsal J, Olsson P, Ohlsson B, Andréasson K. Severe intestinal dysbiosis is prevalent in primary Sjögren's syndrome and is associated with systemic disease activity. Arthritis Res Ther. 2017;19(1):237. https://doi.org/10.1186/s13075-017-1446-2
Forbes JD, Van Domselaar G, Bernstein CN. The gut microbiota in immune-mediated inflammatory diseases. Front Microbiol. 2016;7(JUL):1-2. https://doi.org/10.3389/fmicb.2016.01081
Hayakawa T, Naruse S, Kitagawa M, Kondo T. Clinical aspects of autoimmune pancreatitis in Sjogren's syndrome. J Pancreas. 2001;2(3):88-92.
Afzelius P, Fallentin EM, Larsen S, Møller S, Schiødt M. Pancreatic function and morphology in Sjögren's syndrome. Scand J Gastroenterol. 2010;45(6):752-8. https://doi.org/10.3109/00365521003642542
Skopouli FN, Barbatis C, Moutsopoulos HM. Liver involvement in primary sjögren's syndrome. Rheumatology. 1994;33(8):745-8. https://doi.org/10.1093/rheumatology/33.8.745
Tsianos E V., Hoofnagle JH, Fox PC, Alspaugh M, Jones EA, Schafer DF, et al. Sjögren's syndrome in patients with primary biliary cirrhosis. Hepatology. 1990;11(5):730-4. https://doi.org/10.1002/hep.1840110504
Teufel A, Weinmann A, Kahaly GJ, Centner C, Piendl A, Wörns M, et al. Concurrent autoimmune diseases in patients with autoimmune hepatitis. J Clin Gastroenterol. 2010;44(3):208-13. https://doi.org/10.1097/MCG.0b013e3181c74e0d
Lindor KD, Kowdley K V., Harrison ME. ACG clinical guideline: Primary sclerosing cholangitis. Am J Gastroenterol. 2015;110(5):646-59. https://doi.org/10.1038/ajg.2015.112
Martin P, Dimartini A, Feng S, Brown R, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59(3):1144-65. https://doi.org/10.1002/hep.26972
Haddad J, Trinchet JC, Pateron D, Mal F, Beaugrand M, Munz-Gotheil C, et al. Lymphocytic sialadenitis of Sjögren's syndrome associated with chronic hepatitis C virus liver disease. Lancet. 1992;339(8789):321-3. https://doi.org/10.1016/0140-6736(92)91645-O
Ramos-Casals M, García-Carrasco M, Cervera R, Font J. Sjogren's syndrome and hepatitis C virus. Clin Rheumatol. 1999;18(2):93-100. https://doi.org/10.1007/s100670050064
Aabakken L, Karlsen TH, Albert J, Arvanitakis M, Chazouilleres O, Dumonceau JM, et al. Role of endoscopy in primary sclerosing cholangitis: European Society of Gastrointestinal Endoscopy (ESGE) and European Association for the Study of the Liver (EASL) Clinical Guideline. Endoscopy. 2017;49(6):588-608. https://doi.org/10.1055/s-0043-107029
Dave M, Elmunzer BJ, Dwamena BA, Higgins PDR. Primary sclerosing cholangitis: Meta-analysis of diagnostic performance of MR cholangiopancreatography. Radiology. 2010;256(2):387-96. https://doi.org/10.1148/radiol.10091953
Angulo P, Peter JB, Gershwin ME, DeSotel CK, Shoenfeld Y, Ahmed AEE, et al. Serum autoantibodies in patients with primary sclerosing cholangitis. J Hepatol. 2000;32(2):182-7. https://doi.org/10.1016/S0168-8278(00)80061-6
Hirano K, Kawabe T, Yamamoto N, Nakai Y, Sasahira N, Tsujino T, et al. Serum IgG4 concentrations in pancreatic and biliary diseases. Clin Chim Acta. 2006;367(1-2):181-4. https://doi.org/10.1016/j.cca.2005.11.031
Mendes FD, Jorgensen R, Keach J, Katzmann JA, Smyrk T, Donlinger J, et al. Elevated serum IgG4 concentration in patients with primary sclerosing cholangitis. Am J Gastroenterol. 2006;101(9):2070-5. https://doi.org/10.1111/j.1572-0241.2006.00772.x
Hernández-Molina G, Michel-Peregrina ML. Afección pancreática en el síndrome de sjögren. Reumatol Clin. 2011;7(2):130-4. https://doi.org/10.1016/j.reuma.2010.07.005
Guerrero P, Martín M, Conde JM, Castro M, Rodríguez MC, Castilla L, et al. [Primary segmental sclerosing cholangitis associated with Sjögren's syndrome]. Rev Esp enfermedades Dig organo Of la Soc Esp Patol Dig. 1991;79(5):363-6.
Karlsen TH, Schrumpf E, Boberg KM. Primary sclerosing cholangitis. Best Pract Res Clin Gastroenterol. 2010;24(5):655-66. https://doi.org/10.1016/j.bpg.2010.07.005
Scofield RH. Vasculitis in Sjögren's syndrome. Curr Rheumatol Rep. 2011;13(6):482-8. https://doi.org/10.1007/s11926-011-0207-5
Floreani A, Rizzotto ER, Ferrara F, Carderi I, Caroli D, Blasone L, et al. Clinical course and outcome of autoimmune hepatitis/primary sclerosing cholangitis overlap syndrome. Am J Gastroenterol. 2005;100(7):1516-22.
https://doi.org/10.1111/j.1572-0241.2005.41841.x
Triantos CK, Koukias NM, Nikolopoulou VN, Burroughs AK. Meta-analysis: Ursodeoxycholic acid for primary sclerosing cholangitis. Aliment Pharmacol Ther. 2011;34(8):901-10. https://doi.org/10.1111/j.1365-2036.2011.04822.x
Chapman R, Fevery J, Kalloo A, Nagorney DM, Boberg KM, Shneider B, et al. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010;51(2):660-78. https://doi.org/10.1002/hep.23294
Saffioti F, Gurusamy KS, Hawkins N, Toon CD, Tsochatzis E, Davidson BR, et al. Pharmacological interventions for primary sclerosing cholangitis. Cochrane Database Syst Rev. 2017;2017(4):3-5. https://doi.org/10.1002/14651858.CD011343.pub2
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |