Sedation Administered by General Practitioners for Low Complexity Endoscopic Procedures: Experience in an Endoscopy Unit of a Tertiary Referral Hospital in Cali
DOI:
https://doi.org/10.22516/25007440.836Keywords:
Endoscopy, Colonoscopy, Sedation, general practitioner, Safety, experienceAbstract
Objectives: in Colombia, sedation by non-anesthesiologists for endoscopic procedures outside the operating room has been implemented. A description of an experience in the gastroenterology unit of a tertiary referral hospital in Cali, Colombia, was conducted.
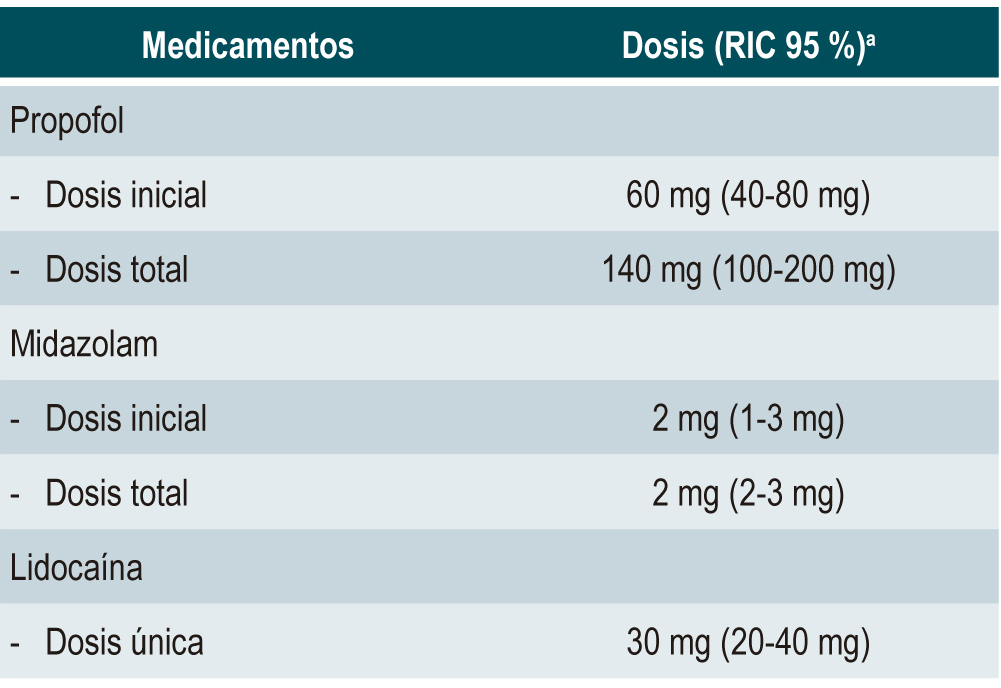
Materials and methods: an analytical cohort observational study to describe the frequency and type of adverse events associated with sedation procedures performed by general practitioners and evaluate the factors related to their occurrence in patients who attended the endoscopy unit of Fundación Valle del Lili for endoscopic studies under intravenous sedation. Between November 2018 and June 2019, non-anesthesiologist physicians performed this procedure due to the minimal risk implied. A descriptive analysis was completed, and the median and interquartile range were calculated for numerical variables and frequencies for qualitative variables.
Results: There were 1506 participants, 59.4% ASA I and 40.6% ASA II in this study. On average, the starting dose of propofol was 60 mg, and the total dose was 140 mg. Forty-six patients (3.05%) reported non-severe adverse events; the most common occurrence was transient desaturation (80.4%). No patients experienced severe adverse events. The average initial Aldrete scale score was 8, while at discharge, the average score was 10.
Conclusions: sedation for endoscopic procedures performed by non-anesthesiologists is safe provided that it is performed by trained personnel conducting a correct assessment of the patient’s (cardiovascular, gastrointestinal, and neurological) history and risk factors within the framework of the current institutional guidelines.
Downloads
References
Saklad M. Grading of patients for surgical procedures. Anesthesiology. 1941;2(3):281-4. https://doi.org/10.1097/00000542-194105000-00004
Mallampati SR, Stephen P, Gugino LD, Desai SP, Crna BW. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J. 1985;32(4):429-34. https://doi.org/10.1007/BF03011357
Aldrete JA. Criterios para dar de alta el puntaje de recuperación post anestésica. Rev Colomb Anestesiol. 1996;24(3):305-12.
Ferreira AO, Torres J, Barjas E, Nunes J, Glória L, Ferreira R, et al. Non-anesthesiologist administration of propofol sedation for colonoscopy is safe in low risk patients: Results of a noninferiority randomized controlled trial. Endoscopy. 2016;48(8):747-53. https://doi.org/10.1055/s-0042-105560
Triantafillidis JK, Merikas E, Nikolakis D, Papalois AE. Sedation in gastrointestinal endoscopy: Current issues. World J Gastroenterol. 2013;19(4):463-81. https://doi.org/10.3748/wjg.v19.i4.463
Khiani VS, Soulos P, Gancayco J, Gross CP. Anesthesiologist involvement in screening colonoscopy: Temporal trends and cost implications in the medicare population. Clin Gastroenterol Hepatol. 2012;10(1):58-64.e1. https://doi.org/10.1016/j.cgh.2011.07.005
Hassan C, Rex DK, Cooper GS, Benamouzig R. Endoscopist-directed propofol administration versus anesthesiologist assistance for colorectal cancer screening: A cost-effectiveness analysis. Endoscopy. 2012;44(5):456-61. https://doi.org/10.1055/s-0032-1308936
Dumonceau JM, Riphaus A, Schreiber F, Vilmann P, Beilenhoff U, Aparicio JR, et al. Non-anesthesiologist administration of propofol for gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates Guideline - Updated June 2015. Endoscopy. 2015;47(12):1175-89. https://doi.org/10.1055/s-0034-1393414
Vargo J, Cohen L, Rex D. Position statement: nonanesthesiologist administration of propofol for GI endoscopy. Gastrointest Endosc. 2009;70(6):1053-9. https://doi.org/10.1016/j.gie.2009.07.020
Ministerio de Salud y Protección Social. Resolución Número 1441 De 2013: Por la cual se definen los procedimientos y condiciones que deben cumplir los Prestadores de Servicios de Salud para habilitar los servicios y se dictan otras disposiciones. 2013.
Burbano-paredes CC, Amaya-guio J, Rubiano-pinzón AM, Hernández-caicedo ÁC. Guía de práctica clínica para la administración de sedación fuera del quirófano en pacientes mayores de 12 años. Rev Colomb Anestesiol. 2017;5(3):224-38. https://doi.org/10.1016/j.rca.2017.02.008
Vargo JJ, Niklewski PJ, Williams JL, Martin JF, Faigel DO. Patient safety during sedation by anesthesia professionals during routine upper endoscopy and colonoscopy: an analysis of 1.38 million procedures. Gastrointest Endosc. 2017;85(1):101-8. https://doi.org/10.1016/j.gie.2016.02.007
Ibarra P, Galindo M, Molano A, Niño C, Rubiano A, Echeverry P, et al. Recomendaciones para la sedación y la analgesia por médicos no anestesiólogos y odontólogos de pacientes mayores de 12 años. Rev Colomb Anestesiol. 2012;40(1):67-74. https://doi.org/10.1016/S0120-3347(12)70012-6
Mullet-Vásquez E, Osorio-chica M, Arango-Molano L. Sedación con propofol por no anestesiólogos para colonoscopia total. Rev Colomb Gastroenterol. 2019;34(4):345-9. https://doi.org/10.22516/25007440.302
Cohen LB, Wecsler JS, Gaetano JN, Benson AA, Miller KM, Durkalski V, et al. Endoscopic Sedation in the United States: Results from a Nationwide Survey. Am J Gastroenterol. 2006;101(5):967-74. https://doi.org/10.1111/j.1572-0241.2006.00500.x
Wadhwa V, Issa D, Garg S, Lopez R, Sanaka MR, Vargo JJ. Similar Risk of Cardiopulmonary Adverse Events Between Propofol and Traditional Anesthesia for Gastrointestinal Endoscopy: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2017;15(2):194-206. https://doi.org/10.1016/j.cgh.2016.07.013
Igea F, Casellas JA, González-Huix F, Gómez-Oliva C, Baudet JS, Cacho G, et al. Sedación en endoscopia digestiva: Guía de práctica clínica de la Sociedad Española de Endoscopia Digestiva. Rev Esp Enfermedades Dig. 2014;106(3):195-211.
Behrens A, Kreuzmayr A, Manner H, Koop H, Lorenz A, Schaefer C, et al. Acute sedation-associated complications in GI endoscopy (ProSed 2 Study): results from the prospective multicentre electronic registry of sedation-associated complications. Gut. 2019;68(3):445-452. https://doi.org/10.1136/gutjnl-2015-311037
Sharma VK, Nguyen CC, Crowell MD, Lieberman DA, de Garmo P, Fleischer DE. A national study of cardiopulmonary unplanned events after GI endoscopy. Gastrointest Endosc. 2007;66(1):27-34. https://doi.org/10.1016/j.gie.2006.12.040
Dossa F, Megetto O, Yakubu M, Zhang DDQ, Baxter NN. Sedation practices for routine gastrointestinal endoscopy: a systematic review of recommendations. BMC Gastroenterol. 2021;21(1):22. https://doi.org/10.1186/s12876-020-01561-z
Gotoda T, Akamatsu T, Abe S, Shimatani M, Nakai Y, Hatta W, et al. Guidelines for sedation in gastroenterological endoscopy (second edition). Dig Endosc. 2021;33(1):21-53. https://doi.org/10.1111/den.13882
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














