Association Between Body Mass Index and Liver Fibrosis Degree Measured Using Real-Time Elastography (Supersonic)
DOI:
https://doi.org/10.22516/25007440.769Keywords:
Non-alcoholic fatty liver, hepatic fibrosis, Cirrhosis, Real-time elastography (supersonic)Abstract
Introduction: Non-alcoholic fatty liver disease (NAFLD) or fatty liver, is characterized by an excessive accumulation of fat in the liver, is a metabolic disorder with a worldwide prevalence close to 25%, with a spectrum of liver damage that covers the steatosis without fibrosis, steatohepatitis with variable fibrosis and cirrhosis or maximum degree of fibrosis, this fibrosis determines prognosis and outcomes in the disease.
Objective: To evaluate the association between body mass index and the degree of liver fibrosis in patients diagnosed with fatty liver in a hepatology center in the city of Bogotá, Colombia.
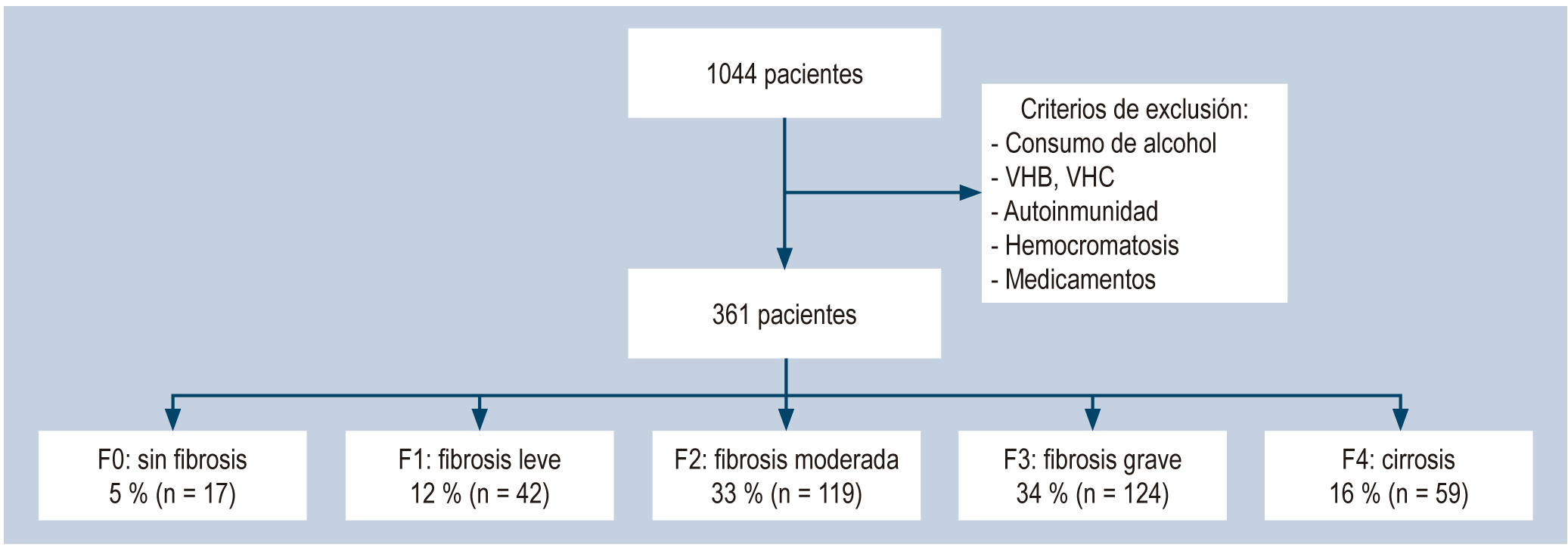
Patients and methods: A case-control study is carried out with patients diagnosed with fatty liver, who have undergone real-time elastography (Supersonic). Information was taken from patients diagnosed with fatty liver who met the inclusion criteria. Continuous variables were described using measures of central tendency and standard deviation. Categorical variables were described with numbers and percentages. A 95% confidence interval was considered statistically significant.
Results: 361 patients were included, of which 95.2% (n=344) presented some degree of alteration (12% minimal fibrosis, 33% moderate fibrosis, 34% severe fibrosis and 16% cirrhosis) and only 5% showed a liver normal. Not having an adequate weight is related to severe fibrosis F3 OR 3.24 (1.03-10) and cirrhosis F4 OR 2.33 (2.33-42.99). No statistically significant differences were found between altered body mass index and any degree of fibrosis OR 2.74 (0.90-8.40). The presence of DM presents a 10-fold risk probability of ending in F4 cirrhosis, especially with poor disease control OR 5.16 (1.23-30.33).
Conclusion: There is an association between abnormal body mass index and glycemic profile and the development of severe and advanced fibrosis. It is necessary in clinical practice, greater surveillance and evaluation of patients with fatty liver, in order to prevent the progression of fibrosis.
Downloads
References
Soresi M, Giannitrapani L, Noto D, Terranova A, Campagna ME, Cefalù AB, et al. Effects of steatosis on hepatic hemodynamics in patients with metabolic syndrome. Ultrasound Med Biol. 2015;41(6):1545-52. https://doi.org/10.1016/j.ultrasmedbio.2015.01.020
European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the Management of Non-Alcoholic Fatty Liver Disease. Obes Facts. 2016;9(2):65-90. https://doi.org/10.1159/000443344
Watanabe S, Hashimoto E, Ikejima K, Uto H, Ono M, Sumida Y, et al. Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. J Gastroenterol. 2015;50(4):364-77. https://doi.org/10.1007/s00535-015-1050-7
Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129(1):113-21. https://doi.org/10.1053/j.gastro.2005.04.014
Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116(6):1413-9. https://doi.org/10.1016/S0016-5085(99)70506-8
Ratziu V, Bonyhay L, Di Martino V, Charlotte F, Cavallaro L, Sayegh-Tainturier MH, et al. Survival, liver failure, and hepatocellular carcinoma in obesity-related cryptogenic cirrhosis. Hepatology. 2002;35(6):1485-93. https://doi.org/10.1053/jhep.2002.33324
Hui JM, Kench JG, Chitturi S, Sud A, Farrell GC, Byth K, et al. Long-term outcomes of cirrhosis in nonalcoholic steatohepatitis compared with hepatitis C. Hepatology. 2003;38(2):420-7. https://doi.org/10.1053/jhep.2003.50320
Ratziu V, Charlotte F, Heurtier A, Gombert S, Giral P, Bruckert E, et al. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology. 2005;128(7):1898-906. https://doi.org/10.1053/j.gastro.2005.03.084
Cholongitas E, Senzolo M, Standish R, Marelli L, Quaglia A, Patch D, et al. A systematic review of the quality of liver biopsy specimens. Am J Clin Pathol. 2006;125(5):710-21. https://doi.org/10.1309/W3XCNT4HKFBN2G0B
Caballería Rovira L, Torán Montserrat P, Auladell Llorens MA, Pera Blanco G. Esteatosis hepática no alcohólica. puesta al día. Atención Primaria. 2008;40(8):419-24. https://doi.org/10.1157/13125408
Wai CT, Greenson JK, Fontana RJ, Kalbfleisch JD, Marrero JA, Conjeevaram HS, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003;38(2):518-26. https://doi.org/10.1053/jhep.2003.50346
Williams AL, Hoofnagle JH. Ratio of serum aspartate to alanine aminotransferase in chronic hepatitis. Relationship to cirrhosis. Gastroenterology. 1988;95(3):734-9. https://doi.org/10.1016/S0016-5085(88)80022-2
Yoshioka K, Hashimoto S, Kawabe N. Measurement of liver stiffness as a non-invasive method for diagnosis of non-alcoholic fatty liver disease. Hepatol Res. 2015;45(2):142-51. https://doi.org/10.1111/hepr.12388
Muller M, Gennisson JL, Deffieux T, Tanter M, Fink M. Quantitative viscoelasticity mapping of human liver using supersonic shear imaging: preliminary in vivo feasibility study. Ultrasound Med Biol. 2009;35(2):219-29. https://doi.org/10.1016/j.ultrasmedbio.2008.08.018
Rodríguez-Ortiz D, Reyes-Pérez A, León P, Sánchez H, Mosti M, Aguilar-Salinas CA, et al. Assessment of two different diagnostic guidelines criteria (National Cholesterol Education Adult Treatment Panel III [ATP III] and International Diabetes Federation [IDF]) for the evaluation of metabolic syndrome remission in a longitudinal cohort of patients undergoing Roux-en-Y gastric bypass. Surgery. 2016;159(4):1121-8. https://doi.org/10.1016/j.surg.2015.11.015
Krakoff LR, Gillespie RL, Ferdinand KC, Fergus IV, Akinboboye O, Williams KA, et al. 2014 hypertension recommendations from the eighth joint national committee panel members raise concerns for elderly black and female populations. J Am Coll Cardiol. 2014;64(4):394-402. https://doi.org/10.1016/j.jacc.2014.06.014
Kuczmarski RJ, Flegal KM. Criteria for definition of overweight in transition: background and recommendations for the United States. Am J Clin Nutr. 2000;72(5):1074-81. https://doi.org/10.1093/ajcn/72.5.1074
Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, Grundy SM, Hobbs HH. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40(6):1387-95. https://doi.org/10.1002/hep.20466
Hashimoto E, Tokushige K. Prevalence, gender, ethnic variations, and prognosis of NASH. J Gastroenterol. 2011;46 Suppl 1:63-9. https://doi.org/10.1007/s00535-010-0311-8
Musso G, Gambino R, Cassader M, Pagano G. Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med. 2011;43(8):617-49. https://doi.org/10.3109/07853890.2010.518623
Serfaty L, Lemoine M. Definition and natural history of metabolic steatosis: clinical aspects of NAFLD, NASH and cirrhosis. Diabetes Metab. 2008;34(6 Pt 2):634-7. https://doi.org/10.1016/S1262-3636(08)74597-X
Eguchi Y, Hyogo H, Ono M, Mizuta T, Ono N, Fujimoto K, et al. Prevalence and associated metabolic factors of nonalcoholic fatty liver disease in the general population from 2009 to 2010 in Japan: a multicenter large retrospective study. J Gastroenterol. 2012;47(5):586-95. https://doi.org/10.1007/s00535-012-0533-z
Leite NC, Salles GF, Araujo AL, Villela-Nogueira CA, Cardoso CR. Prevalence and associated factors of non-alcoholic fatty liver disease in patients with type-2 diabetes mellitus. Liver Int. 2009;29(1):113-9. https://doi.org/10.1111/j.1478-3231.2008.01718.x
Fracanzani AL, Valenti L, Bugianesi E, Andreoletti M, Colli A, Vanni E, et al. Risk of severe liver disease in nonalcoholic fatty liver disease with normal aminotransferase levels: a role for insulin resistance and diabetes. Hepatology. 2008;48(3):792-8. https://doi.org/10.1002/hep.22429
Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346(16):1221-31. https://doi.org/10.1056/NEJMra011775
Angelico F, Del Ben M, Conti R, Francioso S, Feole K, Maccioni D, et al. Non-alcoholic fatty liver syndrome: a hepatic consequence of common metabolic diseases. J Gastroenterol Hepatol. 2003;18(5):588-94. https://doi.org/10.1046/j.1440-1746.2003.02958.x
Kotronen A, Juurinen L, Hakkarainen A, Westerbacka J, Cornér A, Bergholm R, et al. Liver fat is increased in type 2 diabetic patients and underestimated by serum alanine aminotransferase compared with equally obese nondiabetic subjects. Diabetes Care. 2008;31(1):165-9. https://doi.org/10.2337/dc07-1463
Mofrad P, Contos MJ, Haque M, Sargeant C, Fisher RA, Luketic VA, et al. Clinical and histologic spectrum of nonalcoholic fatty liver disease associated with normal ALT values. Hepatology. 2003;37(6):1286-92. https://doi.org/10.1053/jhep.2003.50229
Rahman RN, Ibdah JA. Nonalcoholic fatty liver disease without cirrhosis is an emergent and independent risk factor of hepatocellular carcinoma: A population based study. Hepatology. 2012;56:241A.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














