Survival in Patients with Cirrhosis According to Etiology. Retrospective Cohort
DOI:
https://doi.org/10.22516/25007440.703Keywords:
Survival, Fatty Liver, Non-Alcoholic Fatty Liver Disease, Liver cirrhosisAbstract
Introduction: Cirrhosis is the final stage of chronically progressive liver diseases of various etiologies. It is a common disease, with a variable prevalence in each country. Its peak incidence occurs between 40 and 50 years of age, predominantly in men.
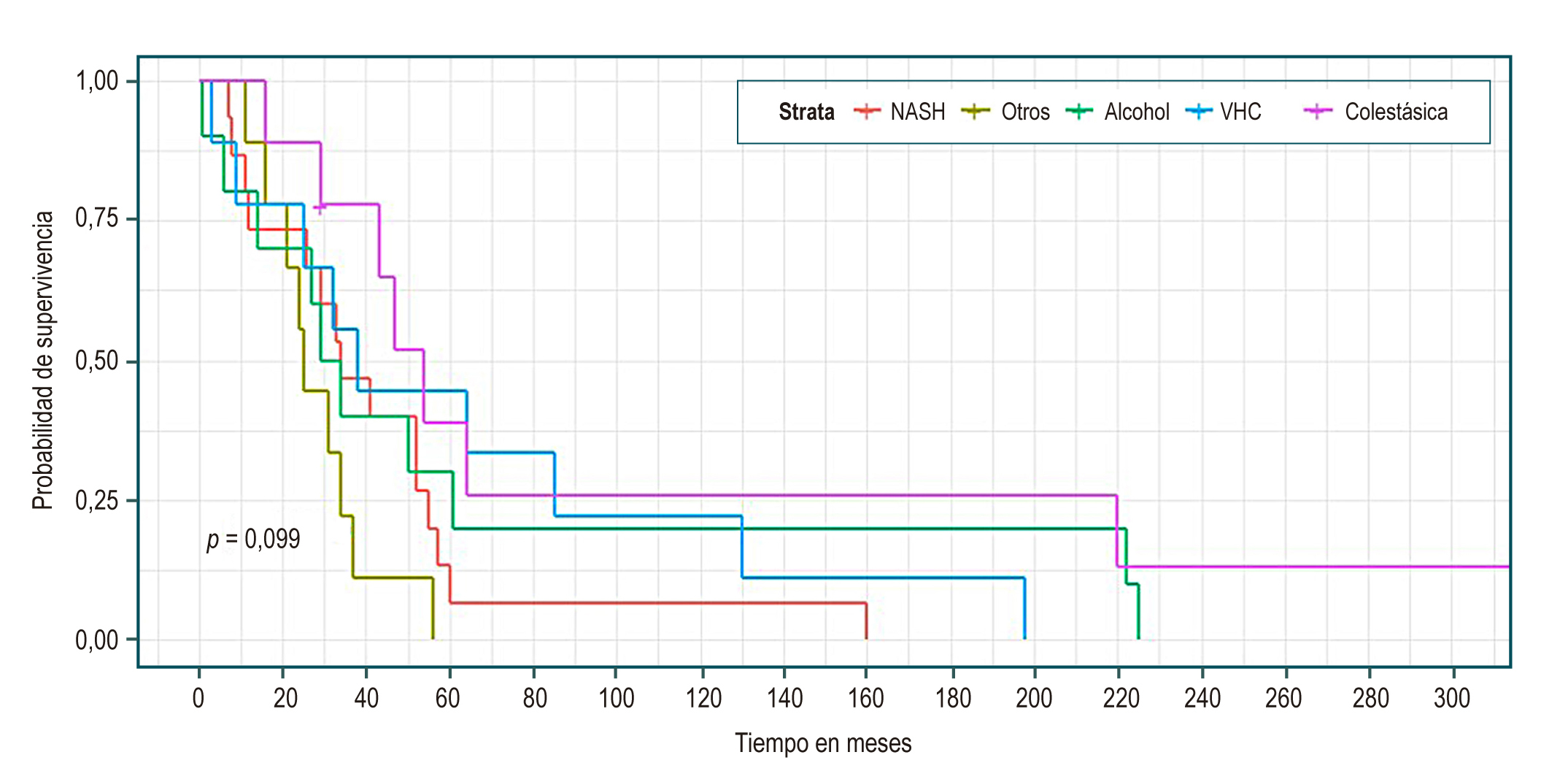
Aims: To compare a cohort of patients diagnosed with cirrhosis, evaluate their complications and survival according to etiology, describe clinical and laboratory aspects, and determine the role of a fatty liver.
Materials and methods: A retrospective cohort study was carried out with patients who held a specialized hepatology consultation in the center of liver and digestive diseases (CEHYD) in Bogotá, Colombia, between January 2010 and June 2019.
Results: We reviewed a total of 1,200 medical records (56.8 % women). There were no statistically significant differences in median survival between groups by etiology, sex, presence or absence of complications, or Child. We noted that the older the age at the diagnosis of cirrhosis, the higher the risk of death; HR 1.04 (95 % CI 1.02-1.075). For each month that follow-up increases, the risk of death decreases by 90 %; HR 0.1 (95 % CI 0.03-0.29). For each month that the follow-up of complications increases, the risk of death is reduced by 2 %; HR 0.98 (95 % CI 0.97-0.99).
Conclusions: Survival by etiology was similar in the different groups. Nonalcoholic steatohepatitis (NASH) was the leading cause of cirrhosis in this cohort. Efforts should focus on its diagnosis and management in the early stages.
Downloads
References
Tsochatzis EA, Bosch J, Burroughs AK. Liver cirrhosis. Lancet. 2014;383(9930):1749-61. https://doi.org/10.1016/S0140-6736(14)60121-5
Lefton HB, Rosa A, Cohen M. Diagnosis and epidemiology of cirrhosis. Med Clin North Am. 2009;93(4):787-99. https://doi.org/10.1016/j.mcna.2009.03.002
Hatzakis A, Wait S, Bruix J, Buti M, Carballo M, Cavaleri M, et al. The state of hepatitis B and C in Europe: Report from the hepatitis B and C summit conference. J Viral Hepat. 2011:18(Suppl 1):1-16. https://doi.org/10.1111/j.1365-2893.2011.01499.x
Anthony PP, Ishak KG, Nayak NC, Poulsen HE, Scheuer PJ, Sobin LH. The morphology of cirrhosis. Recommendations on definition, nomenclature, and classification by a working group sponsored by the World Health Organization. J Clin Pathol. 1978;31(5):395-414. https://doi.org/10.1136/jcp.31.5.395
Lee UE, Friedman SL. Mechanisms of hepatic fibrogenesis. Best Pract Res Clin Gastroenterol. 2011;25(2):195-206. https://doi.org/10.1016/j.bpg.2011.02.005
Friedman SL. Mechanisms of hepatic fibrogenesis. Gastroenterology. 2008;134(6):1655-69. https://doi.org/10.1053/j.gastro.2008.03.003
García-Tsao G, Friedman S, Iredale J, Pinzani M. Now there are many (stages) where before there was one: In search of a pathophysiological classification of cirrhosis. Hepatology. 2010;51(4):1445-9. https://doi.org/10.1002/hep.23478
Desmet VS, Roskams T. Cirrhosis reversal: A duel between dogma and myth. J Hepatol. 2004;40(5):860-7. https://doi.org/10.1016/j.jhep.2004.03.007
Friedman SL, Bansal MB. Reversal of hepatic fibrosis-fact or fantasy? Hepatology. 2006;43(2 Suppl 1):S82-8. https://doi.org/10.1002/hep.20974
Benvegnù L, Gios M, Boccato S, Alberti A. Natural history of compensated viral cirrhosis: A prospective study on the incidence and hierarchy of major complications. Gut. 2004;53(5):744-9. https://doi.org/10.1136/gut.2003.020263
Asrani SK, Kamath PS. Natural history of cirrhosis. Curr Gastroenterol Rep. 2013;15(2):308. https://doi.org/10.1007/s11894-012-0308-y
D’Amico G, García-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: A systematic review of 118 studies. J Hepatol. 2006;44(1):217-31. https://doi.org/10.1016/j.jhep.2005.10.013
Schuppan D, Afdhal NH. Liver cirrhosis. Lancet. 2008;371(9615):838-51. https://doi.org/10.1016/S0140-6736(08)60383-9
D’Amico G, Pagliaro L, Bosch J. Pharmacological treatment of portal hypertension: An evidence-based approach. Semin Liver Dis. 1999;19(4):475-505. https://doi.org/10.1055/s-2007-1007133
Nusrat S, Khan MS, Fazili J, Madhoun MF. Cirrhosis and its complications: Evidence based treatment. World J Gastroenterol. 2014;20(18):5442-60. https://doi.org/10.3748/wjg.v20.i18.5442
Starr SP, Raines D. Cirrhosis: Diagnosis, management, and prevention. Am Fam Physician. 2011;84(12):1353-9.
Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001;94(2):153-6. https://doi.org/10.1002/ijc.1440
Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology. 2005;42(5):1208-36. https://doi.org/10.1002/hep.20933
White DL, Kanwal F, El-Serag HB. Association between nonalcoholic fatty liver disease and risk for hepatocellular cancer, based on systematic review. Clin Gastroenterol Hepatol. 2012;10(12):1342-1359.e2. https://doi.org/10.1016/j.cgh.2012.10.001
Bruix J. Hepatocellular carcinoma: Paving the road for further developments. Semin Liver Dis. 2014;34(4):361. https://doi.org/10.1055/s-0034-1395181
Bose SK, Ray R. Hepatitis C virus infection and insulin resistance. World J Diabetes. 2014;5(1):52-8. https://doi.org/10.4239/wjd.v5.i1.52
Adinolfi LE, Gambardella M, Andreana A, Tripodi MF, Utili R, Ruggiero G. Steatosis accelerates the progression of liver damage of chronic hepatitis C patients and correlates with specific HCV genotype and visceral obesity. Hepatology. 2001;33(6):1358-64. https://doi.org/10.1053/jhep.2001.24432
Haga Y, Kanda T, Sasaki R, Nakamura M, Nakamoto S, Yokosuka O. Nonalcoholic fatty liver disease and hepatic cirrhosis: Comparison with viral hepatitis-associated steatosis. World J Gastroenterol. 2015;21(46):12989-95. https://doi.org/10.3748/wjg.v21.i46.12989
Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33(2):464-70. https://doi.org/10.1053/jhep.2001.22172
Asrani SK, Larson JJ, Yawn B, Therneau TM, Kim WR. Underestimation of liver-related mortality in the United States. Gastroenterology. 2013;145(2):375-82.e.2. https://doi.org/10.1053/j.gastro.2013.04.005
Nilsson E, Anderson H, Sargenti K, Lindgren S, Prytz H. Incidence, clinical presentation and mortality of liver cirrhosis in Southern Sweden: a 10-year population-based study, Aliment Pharmacol Ther. 2016;43(12):1330-9. https://doi.org/10.1111/apt.13635
Dam Fialla A, Schaffalitzky de Muckadell OB, Touborg Lassen A. Incidence, etiology and mortality of cirrhosis: A population-based cohort study. Scand J Gastroenterol. 2012;47(6):702-9. https://doi.org/10.3109/00365521.2012.661759
D’Amico G, Morabito A, Pagliaro L, Marubini E. Survival and prognostic indicators in compensated and decompensated cirrhosis. Dig Dis Sci. 1986;31(5):468-75. https://doi.org/10.1007/BF01320309
D’Amico G. Natural history of compensated cirrhosis and varices. En: Boyer TD, Groszmann RJ (editores). Complications of cirrhosis: pathogenesis, consequences and therapy. VA: American Association for the Study of Liver Diseases; 2001. p. 118-23.
Rodríguez-Osorio I, Mena A, Meijide H, Morano L, Delgado M, Cid P, et al. Liver related events and mortality among elderly patients with advanced chronic hepatitis C treated with direct-acting antivirals. PLoS One. 2019;14(6):e0217052. https://doi.org/10.1371/journal.pone.0217052
Wang X, Lin SX, Tao J, Wei XQ, Liu YT, Chen YM, et al. Study of liver cirrhosis over ten consecutive years in Southern China. World J Gastroenterol. 2014;20(37):13546-55. https://doi.org/10.3748/wjg.v20.i37.13546
Orman ES, Roberts A, Ghabril M, Nephew L, Desai A, Patidar K, et al. Trends in characteristics, mortality, and other outcomes of patients with newly diagnosed cirrhosis. JAMA Netw Open. 2019;5;2(6):e196412. https://doi.org/10.1001/jamanetworkopen.2019.6412
Giraldo AM, Barraza M, Villa H, Martínez JW, García G. Caracterización epidemiológica de pacientes con cirrosis en una consulta de gastroenterología en Pereira, Colombia, 2009-2012. Rev Med Risaralda. 2014;20(2):86-94.
Prieto JE, Sánchez S, Prieto RG, Rojas E, González L, Mendivelso F. Características clínicas y descompensación en pacientes con cirrosis hepática atendidos en dos centros de hepatología en la ciudad de Bogotá D.C., 2010-2014. Rev Col Gastroenterol. 2016;31(1):1-8. https://doi.org/10.22516/25007440.66.
Escorcia Charris E, Marrugo Balceiro W. Caracterización epidemiológica y clínica de la cirrosis hepática en un centro regional del caribe colombiano: clínica general del norte. Enero 2012 a marzo 2017. Bioc. 2018;13(1):17-30. https://doi.org/10.18041/2390-0512/bioc..1.2242
Debes JD, Chan J, Balderramo D, Kikuchi L, Gonzalez E, Prieto JE, et al. Hepatocellular carcinoma in South America: Evaluation of risk factors, demographics and therapy. Liver International. 2018;38(1):136-43. https://doi.org/10.1111/liv.13502
Zhou F, Zhou J, Wang W, Zhang XJ, Ji YX, Zhang P, et al. Unexpected rapid increase in the burden of NAFLD in China from 2008 to 2018: A systematic review and meta-analysis. Hepatology. 2019;70(4):1119-33. https://doi.org/10.1002/hep.30702
Younossi ZM, Golabi P, de Avila L, Paik JM, Srishord M, Fukui N, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis. J Hepatol. 2019;71(4):793-801. https://doi.org/10.1016/j.jhep.2019.06.021
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |















