Clinical and epidemiological description of patients with chronic pancreatitis treated at a quaternary care hospital in Cali, 2011-2017
DOI:
https://doi.org/10.22516/25007440.568Keywords:
chronic pancreatitis, epidemiology, abdominal pain, exocrine pancreatic insufficiencyAbstract
Introduction: Chronic pancreatitis (CP) is a progressive inflammation of the pancreas that can lead to irreversible damage and failure. This condition poses great challenges to physicians since its diagnosis can take months or even years. Patient follow-up is often problematic and knowledge about its clinical presentation and epidemiology in Colombia is scarce. This study aims to describe patients with CP treated at a gastroenterology reference center in Cali, Colombia.
Methodology: Cross-sectional study in adult patients with CP confirmed based on clinical and radiological criteria between 2011 and 2017.
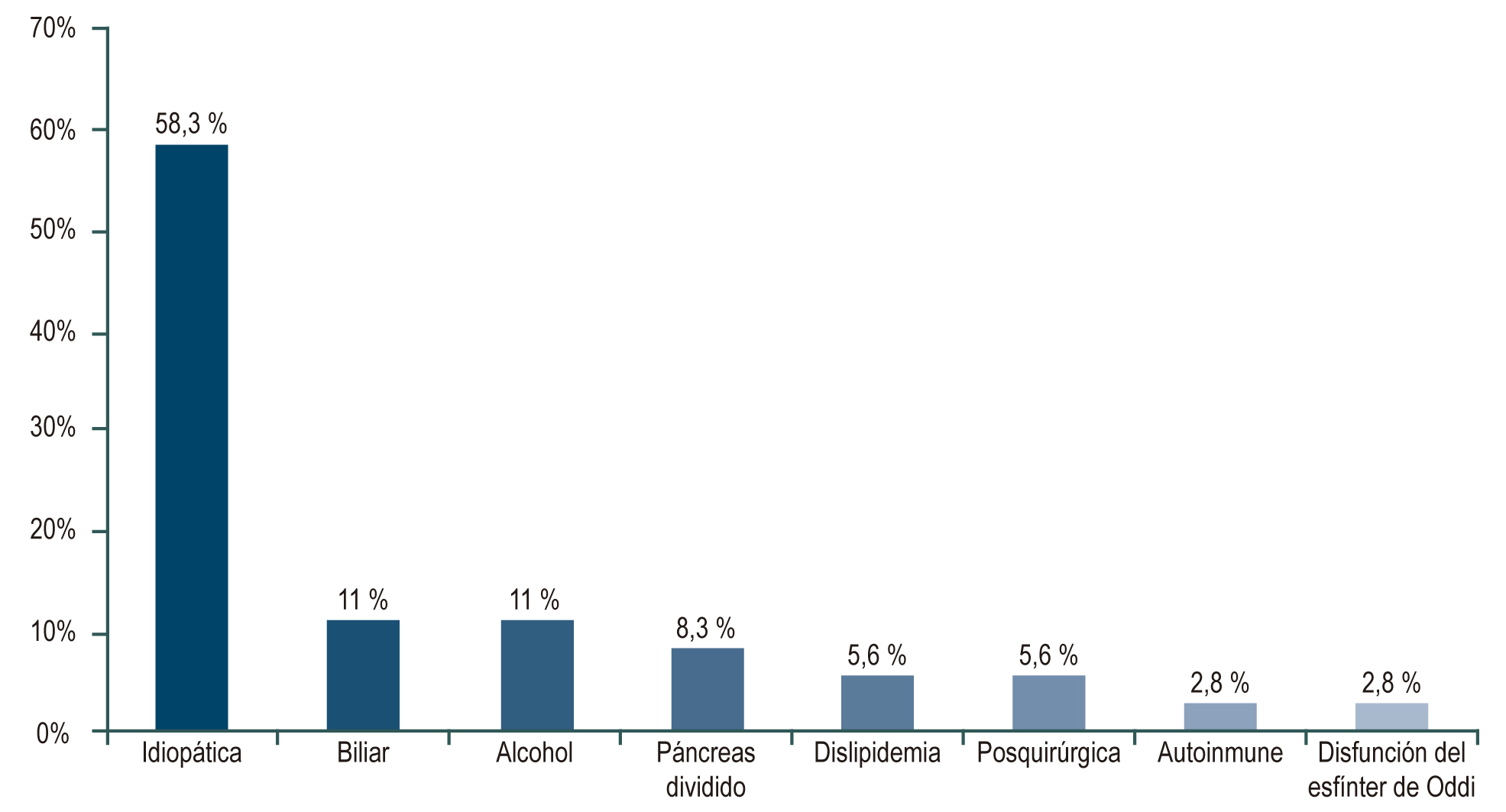
Results: 36 patients with CP were included. The majority were men (72.2 %), and the mean age was 56 (+15.1) years. Chronic abdominal pain was the most common clinical presentation (83.3%). About a quarter of patients had diabetes mellitus (22.2 %). Etiology was idiopathic in 58.3 %, alcoholic in 11.0 %, and biliary in 11.0 %. Computed tomography (CT), magnetic resonance imaging (MRI), and MRI cholangiopancreatography were the most commonly used diagnostic methods (60.5 %), showing mostly atrophy (53.1 %), duct dilation (49.0 %), and pancreatic calcifications (34.7 %).
Conclusion: Nonspecific symptoms of CP in early stages and its long clinical course favor the underdiagnosis of this condition. The results presented may contribute to the future creation of local clinical scales that guide early radiological and genetic studies to achieve a timely diagnosis and improve the quality of life of these patients.
Downloads
References
Muniraj T, Aslanian HR, Farrell J, Jamidar PA. Chronic pancreatitis, a comprehensive review and update. Part I: epidemiology, etiology, risk factors, genetics, pathophysiology, and clinical features. Dis Mon. 2014;60(12):530-50. https://doi.org/10.1016/j.disamonth.2014.11.002
Steer ML, Waxman I, Freedman S. Chronic pancreatitis. N Engl J Med. 1995;332(22):1482-90. https://doi.org/10.1056/NEJM199506013322206
Arango M LA, Díaz T CP, Caicedo Q CA, Ángel Rodríguez C. Estado actual del diagnóstico y manejo de la pancreatitis crónica. Revista Colombiana de Gastroenterologia. 2019;34:376-84. https://doi.org/10.22516/25007440.301
Whitcomb DC, Frulloni L, Garg P, Greer JB, Schneider A, Yadav D, et al. Chronic pancreatitis: An international draft consensus proposal for a new mechanistic definition. Pancreatology. 2016;16(2):218-24. https://doi.org/10.1016/j.pan.2016.02.001
Shimosegawa T, Kataoka K, Kamisawa T, Miyakawa H, Ohara H, Ito T, et al. The revised Japanese clinical diagnostic criteria for chronic pancreatitis. J Gastroenterol. 2010;45(6):584-91. https://doi.org/10.1007/s00535-010-0242-4
Layer P, Yamamoto H, Kalthoff L, Clain JE, Bakken LJ, DiMagno EP. The different courses of early-and late-onset idiopathic and alcoholic chronic pancreatitis. Gastroenterology. 1994;107(5):1481-7.
https://doi.org/10.1016/0016-5085(94)90553-3
Gardner TB, Adler DG, Forsmark CE, Sauer BG, Taylor JR, Whitcomb DC. ACG Clinical Guideline: Chronic Pancreatitis. Am J Gastroenterol. 2020. https://doi.org/10.14309/ajg.0000000000000535
Singh VK, Yadav D, Garg PK. Diagnosis and Management of Chronic Pancreatitis: A Review. JAMA. 2019;322(24):2422-34. https://doi.org/10.1001/jama.2019.19411
Mullady DK, Yadav D, Amann ST, O'Connell MR, Barmada MM, Elta GH, et al. Type of pain, pain-associated complications, quality of life, disability and resource utilisation in chronic pancreatitis: a prospective cohort study. Gut. 2011;60(1):77-84. https://doi.org/10.1136/gut.2010.213835
Wilcox CM, Yadav D, Ye T, Gardner TB, Gelrud A, Sandhu BS, et al. Chronic pancreatitis pain pattern and severity are independent of abdominal imaging findings. Clin Gastroenterol Hepatol. 2015;13(3):552-60; quiz e28-9. https://doi.org/10.1016/j.cgh.2014.12.020
Malka D, Hammel P, Sauvanet A, Rufat P, O'Toole D, Bardet P, et al. Risk factors for diabetes mellitus in chronic pancreatitis. Gastroenterology. 2000;119(5):1324-32. https://doi.org/10.1053/gast.2000.19286
Lankisch PG, Löhr-Happe A, Otto J, Creutzfeldt W. Natural course in chronic pancreatitis. Pain, exocrine and endocrine pancreatic insufficiency and prognosis of the disease. Digestion. 1993;54(3):148-55.
https://doi.org/10.1159/000201029
Raimondi S, Lowenfels AB, Morselli-Labate AM, Maisonneuve P, Pezzilli R. Pancreatic cancer in chronic pancreatitis; aetiology, incidence, and early detection. Best practice & research Clinical gastroenterology. 2010;24(3):349-58. https://doi.org/10.1016/j.bpg.2010.02.007
Lowenfels AB, Maisonneuve P, DiMagno EP, Elitsur Y, Gates LK, Perrault J, et al. Hereditary pancreatitis and the risk of pancreatic cancer. International Hereditary Pancreatitis Study Group. J Natl Cancer Inst. 1997;89(6):442-6. https://doi.org/10.1093/jnci/89.6.442
Nøjgaard C, Bendtsen F, Becker U, Andersen JR, Holst C, Matzen P. Danish patients with chronic pancreatitis have a four-fold higher mortality rate than the Danish population. Clinical Gastroenterology and Hepatology. 2010;8(4):384-90. https://doi.org/10.1016/j.cgh.2009.12.016
Levy P, Milan C, Pignon JP, Baetz A, Bernades P. Mortality factors associated with chronic pancreatitis. Unidimensional and multidimensional analysis of a medical-surgical series of 240 patients. Gastroenterology. 1989;96(4):1165-72. https://doi.org/10.1016/0016-5085(89)91637-5
Yadav D, Timmons L, Benson JT, Dierkhising RA, Chari ST. Incidence, prevalence, and survival of chronic pancreatitis: a population-based study. The American journal of gastroenterology. 2011;106(12):2192-9. https://doi.org/10.1038/ajg.2011.415 https://doi.org/10.1038/ajg.2011.328
Conwell DL, Lee LS, Yadav D, Longnecker DS, Miller FH, Mortele KJ, et al. American Pancreatic Association Practice Guidelines in Chronic Pancreatitis: evidence-based report on diagnostic guidelines. Pancreas. 2014;43(8):1143-62. https://doi.org/10.1097/MPA.0000000000000237
Yadav D, Whitcomb DC. The role of alcohol and smoking in pancreatitis. Nat Rev Gastroenterol Hepatol. 2010;7(3):131-45. https://doi.org/10.1038/nrgastro.2010.6
Whitcomb DC, Group NAPS. Pancreatitis: TIGAR-O Version 2 Risk/Etiology Checklist With Topic Reviews, Updates, and Use Primers. Clin Transl Gastroenterol. 2019;10(6):e00027. https://doi.org/10.14309/ctg.0000000000000027
Etemad B, Whitcomb DC. Chronic pancreatitis: diagnosis, classification, and new genetic developments. Gastroenterology. 2001;120(3):682-707. https://doi.org/10.1053/gast.2001.22586
Czul F, Coronel E, Donet JA. Una actualización de pancreatitis crónica: artículo de revisión. Revista de Gastroenterología del Perú. 2017;37:146-55.
Seicean A. Endoscopic ultrasound in chronic pancreatitis: where are we now? World J Gastroenterol. 2010;16(34):4253-63. https://doi.org/10.3748/wjg.v16.i34.4253
Issa Y, Kempeneers MA, van Santvoort HC, Bollen TL, Bipat S, Boermeester MA. Diagnostic performance of imaging modalities in chronic pancreatitis: a systematic review and meta-analysis. Eur Radiol. 2017;27(9):3820-44. https://doi.org/10.1007/s00330-016-4720-9
Sahai AV, Mishra G, Penman ID, Williams D, Wallace MB, Hadzijahic N, et al. EUS to detect evidence of pancreatic disease in patients with persistent or nonspecific dyspepsia. Gastrointest Endosc. 2000;52(2):153-9. https://doi.org/10.1067/mge.2000.107910
Lévy P, Domínguez-Muñoz E, Imrie C, Löhr M, Maisonneuve P. Epidemiology of chronic pancreatitis: burden of the disease and consequences. United European Gastroenterol J. 2014;2(5):345-54. https://doi.org/10.1177/2050640614548208
Hirota M, Shimosegawa T, Masamune A, Kikuta K, Kume K, Hamada S, et al. The seventh nationwide epidemiological survey for chronic pancreatitis in Japan: clinical significance of smoking habit in Japanese patients. Pancreatology. 2014;14(6):490-6. https://doi.org/10.1016/j.pan.2014.08.008
Lin Y, Tamakoshi A, Matsuno S, Takeda K, Hayakawa T, Kitagawa M, et al. Nationwide epidemiological survey of chronic pancreatitis in Japan. J Gastroenterol. 2000;35(2):136-41. https://doi.org/10.1007/s005350050026 https://doi.org/10.1007/s005350050034
Nikolic S, Dugic A, Steiner C, Tsolakis AV, Haugen Löfman IM, Löhr JM, et al. Chronic pancreatitis and the heart disease: Still terra incognita? World J Gastroenterol. 2019;25(44):6561-70. https://doi.org/10.3748/wjg.v25.i44.6561
Hsu MT, Lin CL, Chung WS. Increased Risk of Acute Coronary Syndrome in Patients With Chronic Pancreatitis: A Nationwide Cohort Analysis. Medicine (Baltimore). 2016;95(20):e3451. https://doi.org/10.1097/MD.0000000000003451
Gullo L, Stella A, Labriola E, Costa PL, Descovich G, Labò G. Cardiovascular lesions in chronic pancreatitis: a prospective study. Dig Dis Sci. 1982;27(8):716-22. https://doi.org/10.1007/BF01393767
Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144(6):1252-61. https://doi.org/10.1053/j.gastro.2013.01.068
Conwell DL, Banks PA, Sandhu BS, Sherman S, Al-Kaade S, Gardner TB, et al. Validation of Demographics, Etiology, and Risk Factors for Chronic Pancreatitis in the USA: A Report of the North American Pancreas Study (NAPS) Group. Dig Dis Sci. 2017;62(8):2133-40. https://doi.org/10.1007/s10620-017-4621-z
Schneider A, Löhr JM, Singer MV. The M-ANNHEIM classification of chronic pancreatitis: introduction of a unifying classification system based on a review of previous classifications of the disease. J Gastroenterol. 2007;42(2):101-19. https://doi.org/10.1007/s00535-006-1945-4
Hao L, Wang LS, Liu Y, Wang T, Guo HL, Pan J, et al. The different course of alcoholic and idiopathic chronic pancreatitis: A long-term study of 2,037 patients. PLoS One. 2018;13(6):e0198365. https://doi.org/10.1371/journal.pone.0198365
Li BR, Pan J, Du TT, Liao Z, Ye B, Zou WB, et al. Risk Factors for Steatorrhea in Chronic Pancreatitis: A Cohort of 2,153 Patients. Sci Rep. 2016;6:21381. https://doi.org/10.1038/srep21381
Hirota M, Shimosegawa T, Masamune A, Kikuta K, Kume K, Hamada S, et al. The sixth nationwide epidemiological survey of chronic pancreatitis in Japan. Pancreatology. 2012;12(2):79-84. https://doi.org/10.1016/j.pan.2012.02.005
Wilcox CM, Sandhu BS, Singh V, Gelrud A, Abberbock JN, Sherman S, et al. Racial Differences in the Clinical Profile, Causes, and Outcome of Chronic Pancreatitis. Am J Gastroenterol. 2016;111(10):1488-96. https://doi.org/10.1038/ajg.2016.316
Whitcomb DC, Yadav D, Adam S, Hawes RH, Brand RE, Anderson MA, et al. Multicenter approach to recurrent acute and chronic pancreatitis in the United States: the North American Pancreatitis Study 2 (NAPS2). Pancreatology. 2008;8(4-5):520-31. https://doi.org/10.1159/000152001
Yadav D, Hawes RH, Brand RE, Anderson MA, Money ME, Banks PA, et al. Alcohol consumption, cigarette smoking, and the risk of recurrent acute and chronic pancreatitis. Arch Intern Med. 2009;169(11):1035-45. https://doi.org/10.1001/archinternmed.2009.125
Midha S, Khajuria R, Shastri S, Kabra M, Garg PK. Idiopathic chronic pancreatitis in India: phenotypic characterisation and strong genetic susceptibility due to SPINK1 and CFTR gene mutations. Gut. 2010;59(6):800-7. https://doi.org/10.1136/gut.2009.191239
Rosendahl J, Landt O, Bernadova J, Kovacs P, Teich N, Bödeker H, et al. CFTR, SPINK1, CTRC and PRSS1 variants in chronic pancreatitis: is the role of mutated CFTR overestimated? Gut. 2013;62(4):582-92. https://doi.org/10.1136/gutjnl-2011-300645
Zou WB, Tang XY, Zhou DZ, Qian YY, Hu LH, Yu FF, et al. SPINK1, PRSS1, CTRC, and CFTR Genotypes Influence Disease Onset and Clinical Outcomes in Chronic Pancreatitis. Clin Transl Gastroenterol. 2018;9(11):204. https://doi.org/10.1038/s41424-018-0069-5
Pfützer RH, Barmada MM, Brunskill AP, Finch R, Hart PS, Neoptolemos J, et al. SPINK1/PSTI polymorphisms act as disease modifiers in familial and idiopathic chronic pancreatitis. Gastroenterology. 2000;119(3):615-23. https://doi.org/10.1053/gast.2000.18017
Rosendahl J, Witt H, Szmola R, Bhatia E, Ozsvári B, Landt O, et al. Chymotrypsin C (CTRC) variants that diminish activity or secretion are associated with chronic pancreatitis. Nat Genet. 2008;40(1):78-82. https://doi.org/10.1038/ng.2007.44
Whitcomb DC, Gorry MC, Preston RA, Furey W, Sossenheimer MJ, Ulrich CD, et al. Hereditary pancreatitis is caused by a mutation in the cationic trypsinogen gene. Nat Genet. 1996;14(2):141-5. https://doi.org/10.1038/ng1096-141
Luetmer PH, Stephens DH, Ward EM. Chronic pancreatitis: reassessment with current CT. Radiology. 1989;171(2):353-7. https://doi.org/10.1148/radiology.171.2.2704799
Joergensen MT, Brusgaard K, Crüger DG, Gerdes AM, Schaffalitzky de Muckadell OB. Genetic, epidemiological, and clinical aspects of hereditary pancreatitis: a population-based cohort study in Denmark. Am J Gastroenterol. 2010;105(8):1876-83. https://doi.org/10.1038/ajg.2010.193
Catalano MF, Sahai A, Levy M, Romagnuolo J, Wiersema M, Brugge W, et al. EUS-based criteria for the diagnosis of chronic pancreatitis: the Rosemont classification. Gastrointest Endosc. 2009;69(7):1251-61. https://doi.org/10.1016/j.gie.2008.07.043
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |















