Helicobacter pylori susceptibility to six commonly used antibiotics in Colombia
DOI:
https://doi.org/10.22516/25007440.493Keywords:
Helicobacter pylori, Antimicrobial resistance, Gastroduodenal disorders, Gastric cancerAbstract
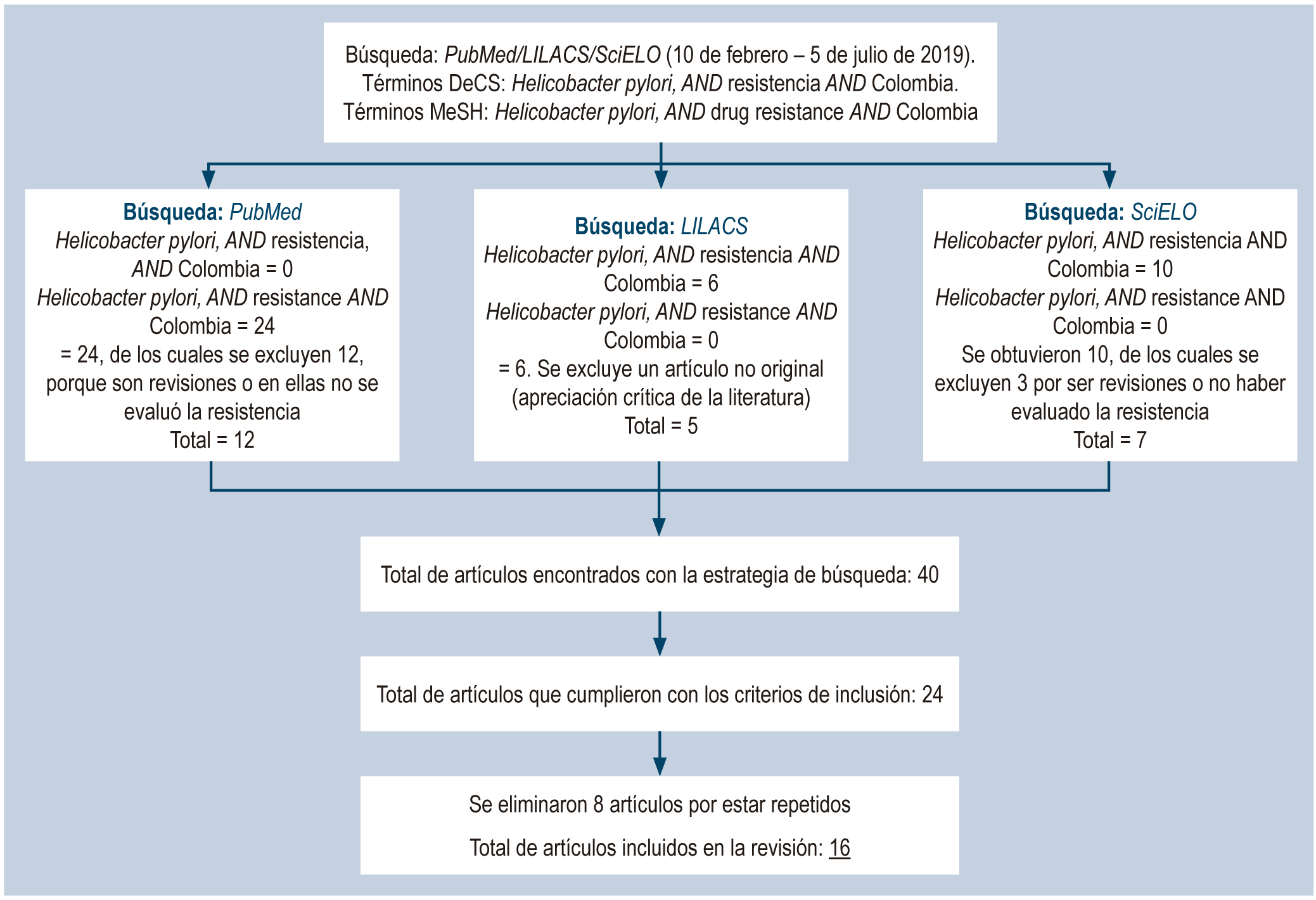
Helicobacter pylori (H. pylori) is a microaerophilic gram-negative bacillus that colonizes the gastric mucosa. It infects more than half the world’s population, making it the most common bacterial infection. The prevalence of infection and associated diseases is high in developing countries. The recommended treatment for its eradication is triple therapy; however, its efficacy has decreased due to the lack of knowledge of the bacterial susceptibility pattern among the medical staff and the emergence of resistant strains. H. pylori susceptibility is associated with the bacteria’s ability to adapt to hostile environments and the use of antibiotics. In Colombia, it has been reported that H. pylori is resistant to amoxicillin, metronidazole, clarithromycin, furazolidone, levofloxacin, and tetracycline. Studies on the susceptibility pattern have determined that the frequency of H. pylori susceptibility is variable and demonstrate the lack of data in most of the Colombian territory. With this in mind, the objective of this review is to describe the percentage of resistance to amoxicillin, metronidazole, clarithromycin, furazolidone, levofloxacin and tetracycline, which are used for the treatment of H. pylori infection, according to studies conducted in Colombia.
Downloads
References
Loughlin MF. Novel therapeutic targets in Helicobacter pylori. Expert Opin Ther Targets. 2003;7(6):725-735. http://doi.org/10.1517/14728222.7.6.725
Kusters JG, van Vliet AH, Kuipers EJ. Pathogenesis of Helicobacter pylori infection. Clin Microbiol Rev. 2006;19(3):449-490.
http://doi.org/10.1128/CMR.00054-05
O’Connor A, O’Morain CA, Ford AC. Population screening and treatment of Helicobacter pylori infection. Nat Rev Gastroenterol Hepatol. 2017;14(4):230-240.
http://doi.org/10.1038/nrgastro.2016.195
Silva GM, Silva HM, Nascimento J, Gonçalves JP, Pereira F, Lima R. Helicobacter pylori antimicrobial resistance in a pediatric population. Helicobacter. 2018;23(5):e12528. http://doi.org/10.1111/hel.12528
Nagy P, Johansson S, Molloy-Bland M. Systematic review of time trends in the prevalence of Helicobacter pylori infection in China and the USA. Gut Pathog. 2016;8:8.
http://doi.org/10.1186/s13099-016-0091-7
Goh KL, Chan WK, Shiota S, Yamaoka Y. Epidemiology of Helicobacter pylori infection and public health implications. Helicobacter. 2011;16 Suppl 1(0 1):1-9.
http://doi.org/10.1111/j.1523-5378.2011.00874.x
Fernández-Delgado M, Contreras M, García-Amado MA, Michelangeli F, Suárez P. Evidencias de la transmisión acuática de Helicobacter pylori. Interciencia. 2008;33(6):412-417.
Gomes BC, de Martinis EC. Fate of Helicobacter pylori artificially inoculated in lettuce and carrot samples. Braz J Microbiol. 2004;35(1):145-150.
https://doi.org/10.1590/S1517-83822004000100024
International Agency for Research on Cancer (IARC). Helicobacter pylori eradication as a strategy for preventing gastric cancer: IARC working group report, volume 8. Lyon: International Agency for Research on Cancer; 2014.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424. http://doi.org/10.3322/caac.21492
IARC Working Group on the Evaluation of Carcinogenic Risk to Humans. Schistosomes, Liver Flukes and Helicobacter pylori. Lyon (FR): International Agency for Research on Cancer; 1994. (IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, No. 61.) Disponible en: https://www.ncbi.nlm.nih.gov/books/NBK487782/
Camargo MC, García A, Riquelme A, Otero W, Camargo CA, Hernández-García T, Candia R, Bruce MG, Rabkin CS. The problem of Helicobacter pylori resistance to antibiotics: a systematic review in Latin America. Am J Gastroenterol. 2014;109(4):485-95.
http://doi.org/10.1038/ajg.2014.24
Malfertheiner P, Megraud F, O’Morain CA, Gisbert JP, Kuipers EJ, Axon AT, Bazzoli F, Gasbarrini A, Atherton J, Graham DY, Hunt R, Moayyedi P, Rokkas T, Rugge M, Selgrad M, Suerbaum S, Sugano K, El-Omar EM; European Helicobacter and Microbiota Study Group and Consensus panel. Management of Helicobacter pylori infection-the Maastricht V/Florence Consensus Report. Gut. 2017;66(1):6-30.
http://doi.org/10.1136/gutjnl-2016-312288
Otero W, Trespalacios AA, Otero L, Vallejo MT, Torres M, Pardo R, Sabbagh L. Guía de práctica clínica para el diagnóstico y tratamiento de la infección por Helicobacter pylori en adultos. Rev Col Gastroenterol. 2015;30 supl. 1:17-33.
Wang D, Guo Q, Yuan Y, Gong Y. The antibiotic resistance of Helicobacter pylori to five antibiotics and influencing factors in an area of China with a high risk of gastric cancer. BMC Microbiol. 2019;19(1):152.
http://doi.org/10.1186/s12866-019-1517-4
Arévalo A, Otero WA, Trespalacios AA. Helicobacter pylori: resistencia múltiple en pacientes de Bogotá, Colombia. Biomédica. 2019;39 supl. 1:125-134.
https://doi.org/10.7705/biomedica.v39i3.4437
Björkholm B, Sjölund M, Falk PG, Berg OG, Engstrand L, Andersson DI. Mutation frequency and biological cost of antibiotic resistance in Helicobacter pylori. Proc Natl Acad Sci U S A. 2001;98(25):14607-14612.
http://doi.org/10.1073/pnas.241517298
Jorgensen M, Daskalopoulos G, Warburton V, Mitchell HM, Hazell SL. Multiple strain colonization and metronidazole resistance in Helicobacter pylori-infected patients: identification from sequential and multiple biopsy specimens. J Infect Dis. 1996;174(3):631-635.
http://doi.org/10.1093/infdis/174.3.631
Enroth H, Björkholm B, Engstrand L. Occurence of resistance mutation and clonal expansion in Helicobacter pylori multiple-strain infection: a potential risk in clarithromycin-based therapy. Clin Infect Dis. 1999;28(6):1305-1307. http://doi.org/10.1086/514796
Otero W, Trespalacios AA, Otero E. Helicobacter pylori: Tratamiento actual, un importante reto en gastroenterología. Rev Col Gastroenterol. 2009;24(3):279-292.
Furuta Y, Konno M, Osaki T, Yonezawa H, Ishige T, Imai M, Shiwa Y, Shibata-Hatta M, Kanesaki Y, Yoshikawa H, Kamiya S, Kobayashi I. Microevolution of Virulence-Related Genes in Helicobacter pylori Familial Infection. PLoS One. 2015;10(5):e0127197.
http://doi.org/10.1371/journal.pone.0127197
Cao Q, Didelot X, Wu Z, Li Z, He L, Li Y, Ni M, You Y, Lin X, Li Z, Gong Y, Zheng M, Zhang M, Liu J, Wang W, Bo X, Falush D, Wang S, Zhang J. Progressive genomic convergence of two Helicobacter pylori strains during mixed infection of a patient with chronic gastritis. Gut. 2015;64(4):554-61.
http://doi.org/10.1136/gutjnl-2014-307345
Suerbaum S, Smith JM, Bapumia K, Morelli G, Smith NH, Kunstmann E, Dyrek I, Achtman M. Free recombination within Helicobacter pylori. Proc Natl Acad Sci U S A. 1998;95(21):12619-24.
http://doi.org/10.1073/pnas.95.21.12619
Andersson DI, Hughes D. Antibiotic resistance and its cost: is it possible to reverse resistance?. Nat Rev Microbiol. 2010;8(4):260-271. http://doi.org/10.1038/nrmicro2319
Tseng YS, Wu DC, Chang CY, Kuo CH, Yang YC, Jan CM, Su YC, Kuo FC, Chang LL. Amoxicillin resistance with beta-lactamase production in Helicobacter pylori. Eur J Clin Invest. 2009;39(9):807-12.
http://doi.org/10.1111/j.1365-2362.2009.02166.x
Binh TT, Suzuki R, Trang TT, Kwon DH, Yamaoka Y. Search for novel candidate mutations for metronidazole resistance in Helicobacter pylori using next-generation sequencing. Antimicrob Agents Chemother. 2015;59(4):2343-2348. http://doi.org/10.1128/AAC.04852-14
Wang LH, Cheng H, Hu FL, Li J. Distribution of gyrA mutations in fluoroquinolone-resistant Helicobacter pylori strains. World J Gastroenterol. 2010;16(18):2272-2277. http://doi.org/10.3748/wjg.v16.i18.2272
Talebi Bezmin Abadi A, Ghasemzadeh A, Taghvaei T, Mobarez AM. Primary resistance of Helicobacter pylori to levofloxacin and moxifloxacine in Iran. Intern Emerg Med. 2012;7(5):447-452.
http://doi.org/10.1007/s11739-011-0563-1
Trespalacios AA, Otero W, Caminos JE, Mercado MM, Avila J, Rosero LE, Arévalo A, Poutou-Piñales RA, Graham DY. Phenotypic and genotypic analysis of clarithromycin-resistant Helicobacter pylori from Bogotá D.C., Colombia. J Microbiol. 2013;51(4):448-52.
http://doi.org/10.1007/s12275-013-2465-6
Mégraud F, Lehours P. Helicobacter pylori detection and antimicrobial susceptibility testing. Clin Microbiol Rev. 2007;20(2):280-322.
http://doi.org/10.1128/CMR.00033-06
Liu ZQ, Zheng PY, Yang PC. Efflux pump gene hefA of Helicobacter pylori plays an important role in multidrug resistance. World J Gastroenterol. 2008;14(33):5217-5222. http://doi.org/10.3748/wjg.14.5217
Dore MP, Sepúlveda AR, Mura I, Realdi G, Osato MS, Graham DY. Explanation for variability of omeprazole amoxycillin therapy? Tolerance of H. pylori to amoxycillin. Gastroenterology.1997;112:A105.
Gómez M, Otero W, Gutiérrez O. Tratamiento de la infección por Helicobacter pylori. Encuesta en un grupo de médicos generales y especialistas en Colombia. Rev Col Gastroenterol. 2007;22(1):7-16.
Yepes CA, Rodríguez A, Ruiz A, Ariza B. Resistencia antibiótica del Helicobacter pylori en el Hospital Universitario San Ignacio de Bogotá. Acta Med Colomb. 2008;33(1):11-14.
Álvarez A, Moncayo JI, Santacruz JJ, Corredor LF, Reinosa E, Martínez JW, Beltrán L. Resistencia a metronidazol y claritromicina en aislamientos de Helicobacter pylori de pacientes dispépticos en Colombia. Red Med Chile. 2009;137(10):1309-1314.
http://dx.doi.org/10.4067/S0034-98872009001000005
Trespalacios AA, Otero W, Mercado M. Resistencia de Helicobacter pylori a metronidazol, claritromicina y amoxicilina en pacientes colombianos. Rev Col Gastroenterol. 2010;25(1):31-38.
Francesco VD, Zullo A, Hassan C, Giorgio F, Rosania R, Ierardi E. Mechanisms of Helicobacter pylori antibiotic resistance: An updated appraisal. World J Gastrointest Pathophysiol. 2011;2(3):35-41.
http://doi.org/10.4291/wjgp.v2.i3.35
Connor A, Vaira D, Gisbert JP, O’Morain C. Treatment of Helicobacter pylori Infection 2014. Helicobacter. 2014;19(1):38-45.
https://doi.org/10.1111/hel.12163
Jenks PJ, Edwards DI. Metronidazole resistance in Helicobacter pylori. Int J Antimicrob Agents. 2002;19(1):1-7.
http://doi.org/10.1016/s0924-8579(01)00468-x
Kim SY, Joo YM, Lee HS, Chung IS, Yoo YJ, Merrell DS, Cha JH. Genetic analysis of Helicobacter pylori clinical isolates suggests resistance to metronidazole can occur without the loss of functional rdxA. J Antibiot (Tokyo). 2009;62(1):43-50.
http://doi.org/10.1038/ja.2008.6
Osato MS, Reddy R, Reddy SG, Penland RL, Graham DY. Comparison of the Etest and the NCCLS-approved agar dilution method to detect metronidazole and clarithromycin resistant Helicobacter pylori. Int J Antimicrob Agents. 2001;17(1):39-44.
http://doi.org/10.1016/s0924-8579(00)00320-4
Acosta CP, Quiroga AJ, Sierra CH, Trespalacios AA. Frecuencia de mutaciones de la nitrorreductasa RdxA de Helicobacter pylori para la activación del metronidazol en una población del departamento del Cauca, Colombia. Biomédica. 2017;37(2):191-199.
https://doi.org/10.7705/biomedica.v37i2.3007
Versalovic J, Shortridge D, Kibler K, Griffy MV, Beyer J, Flamm RK, Tanaka SK, Graham DY, Go MF. Mutations in 23S rRNA are associated with clarithromycin resistance in Helicobacter pylori. Antimicrob Agents Chemother. 1996;40(2):477-80.
http://doi.org/10.1128/AAC.40.2.477
Mégraud F, Corti R. Resistencia bacteriana del Helicobacter pylori en el mundo en el año 2009. Acta Gastroenterol Latinoam. 2009;39(4):282-290.
Schmitt BH, Regner M, Mangold KA, Thomson RB Jr, Kaul KL. PCR detection of clarithromycin-susceptible and -resistant Helicobacter pylori from formalin-fixed, paraffin-embedded gastric biopsies. Mod Pathol. 2013;26(9):1222-1227.
http://doi.org/10.1038/modpathol.2013.48
Agudo S, Pérez-Pérez G, Alarcón T, López-Brea M. High prevalence of clarithromycin-resistant Helicobacter pylori strains and risk factors associated with resistance in Madrid, Spain. J Clin Microbiol. 2010;48(10):3703-3707.
http://doi.org/10.1128/JCM.00144-10
Fontana C, Favaro M, Minelli S, Criscuolo AA, Pietroiusti A, Galante A, Favalli C. New site of modification of 23S rRNA associated with clarithromycin resistance of Helicobacter pylori clinical isolates. Antimicrob Agents Chemother. 2002;46(12):3765-9.
http://doi.org/10.1128/aac.46.12.3765-3769.2002
Hao Q, Li Y, Zhang ZJ, Liu Y, Gao H. New mutation points in 23S rRNA gene associated with Helicobacter pylori resistance to clarithromycin in northeast China. World J Gastroenterol. 2004;10(7):1075-1077.
http://doi.org/10.3748/wjg.v10.i7.1075
Roldán IJ, Castaño R, Navas MC. Mutaciones del gen ARN ribosómico 23S de Helicobacter pylori asociadas con resistencia a claritromicina en pacientes atendidos en una unidad de endoscopia de Medellín, Colombia. Biomédica. 2019;39(supl. 2):117-129.
https://doi.org/10.7705/biomedica.v39i4.4377
Kwon DH, Lee M, Kim JJ, Kim JG, El-Zaatari FA, Osato MS, Graham DY. Furazolidone- and nitrofurantoin-resistant Helicobacter pylori: prevalence and role of genes involved in metronidazole resistance. Antimicrob Agents Chemother. 2001;45(1):306-8.
http://doi.org/10.1128/AAC.45.1.306-308.2001
Su Z, Xu H, Zhang C, Shao S, Li L, Wang H, Wang H, Qiu G. Mutations in Helicobacter pylori porD and oorD genes may contribute to furazolidone resistance. Croat Med J. 2006;47(3):410-5.
Sisson G, Goodwin A, Raudonikiene A, Hughes NJ, Mukhopadhyay AK, Berg DE, Hoffman PS. Enzymes associated with reductive activation and action of nitazoxanide, nitrofurans, and metronidazole in Helicobacter pylori. Antimicrob Agents Chemother. 2002;46(7):2116-23. http://doi.org/10.1128/aac.46.7.2116-2123.2002
Gambia CR, Quevedo NA. Determinación in vitro de la resistencia de Helicobacter pylori a la furazolidona. Bogotá: Facultad de Ciencias, Pontificia Universidad Javeriana; 2009.
Glocker E, Kist M. Rapid detection of point mutations in the gyrA gene of Helicobacter pylori conferring resistance to ciprofloxacin by a fluorescence resonance energy transfer-based real-time PCR approach. J Clin Microbiol. 2004;42(5):2241-2246.
http://doi.org/10.1128/jcm.42.5.2241-2246.2004
Tankovic J, Lascols C, Sculo Q, Petit JC, Soussy CJ. Single and double mutations in gyrA but not in gyrB are associated with low- and high-level fluoroquinolone resistance in Helicobacter pylori. Antimicrob Agents Chemother. 2003;47(12):3942-3944.
http://doi.org/10.1128/aac.47.12.3942-3944.2003
Trespalacios-Rangel AA, Otero W, Arévalo-Galvis A, Poutou-Piñales RA, Rimbara E, Graham DY. Surveillance of Levofloxacin Resistance in Helicobacter pylori Isolates in Bogotá-Colombia (2009-2014). PLoS One. 2016;11(7):e0160007.
http://doi.org/10.1371/journal.pone.0160007
Ribeiro ML, Gerrits MM, Benvengo YH, Berning M, Godoy AP, Kuipers EJ, Mendonça S, van Vliet AH, Pedrazzoli J Jr, Kusters JG. Detection of high-level tetracycline resistance in clinical isolates of Helicobacter pylori using PCR-RFLP. FEMS Immunol Med Microbiol. 2004;40(1):57-61.
http://doi.org/10.1016/S0928-8244(03)00277-3
Gerrits MM, Berning M, Van Vliet AH, Kuipers EJ, Kusters JG. Effects of 16S rRNA gene mutations on tetracycline resistance in Helicobacter pylori. Antimicrob Agents Chemother. 2003;47(9):2984-2986.
http://doi.org/10.1128/aac.47.9.2984-2986.2003
Wu JY, Kim JJ, Reddy R, Wang WM, Graham DY, Kwon DH. Tetracycline-resistant clinical Helicobacter pylori isolates with and without mutations in 16S rRNA-encoding genes. Antimicrob Agents Chemother. 2005;49(2):578-583.
http://doi.org/10.1128/AAC.49.2.578-583.2005
Toledo H, López-Solís R. Tetracycline resistance in Chilean clinical isolates of Helicobacter pylori. J Antimicrob Chemother 2010;65(3):470-473.
https://doi.org/10.1093/jac/dkp457
Lawson AJ, Elviss NC, Owen RJ. Real-time PCR detection and frequency of 16S rDNA mutations associated with resistance and reduced susceptibility to tetracycline in Helicobacter pylori from England and Wales. J Antimicrob Chemother. 2005;56(2):282-286.
http://doi.org/10.1093/jac/dki199
Henao SC, Otero W, Ángel LA, Martínez JD. Resistencia primaria a metronidazol en aislamientos de Helicobacter pylori en pacientes adultos de Bogotá, Colombia. Rev Col Gastroenterol. 2009;24(1):10-15.
Figueroa M, Cortés A, Pazos A, Bravo LE. Sensibilidad in vitro a amoxicilina y claritromicina de Helicobacter pylori obtenido de biopsias gástricas de pacientes en zona de bajo riesgo para cáncer gástrico. Biomédica. 2012;32(1):32-42. https://doi.org/10.7705/biomedica.v32i1.454
Álvarez A, Moncayo JI, Santacruz JJ, Santacoloma M, Corredor LF, Reinosa E. Antimicrobial susceptibility and mutations involved in clarithromycin resistance in Helicobacter pylori isolates from patients in the western central region of Colombia. Antimicrob Agents Chemother. 2009;53(9):4022-4024.
http://doi.org/10.1128/AAC.00145-09
Acosta CP, Hurtado FA, Trespalacios AA. Determinación de mutaciones de un solo nucleótido en el gen 23S rRNA de Helicobacter pylori relacionadas con resistencia a claritromicina en una población del departamento del Cauca, Colombia. Biomédica. 2014;34(Supl. 1):156-62.
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |















