Agreement between Marshall, Ranson and Apache II as estimators of morbidity and mortality in acute pancreatitis
DOI:
https://doi.org/10.22516/25007440.457Keywords:
Acute pancreatitis, Agreement, Mortality, Multivariate prediction modelsAbstract
Introduction: Different scales to estimate the risk of morbidity and mortality in patients with pancreatitis are currently in use in Colombia, which leads to uncertainty when classifying and treating these patients.
Objective: This study seeks to analyze agreement between the most used scales to estimate the risk of patient morbidity and mortality in a population treated at 2,670 meters above sea level (m.a.s.l.).
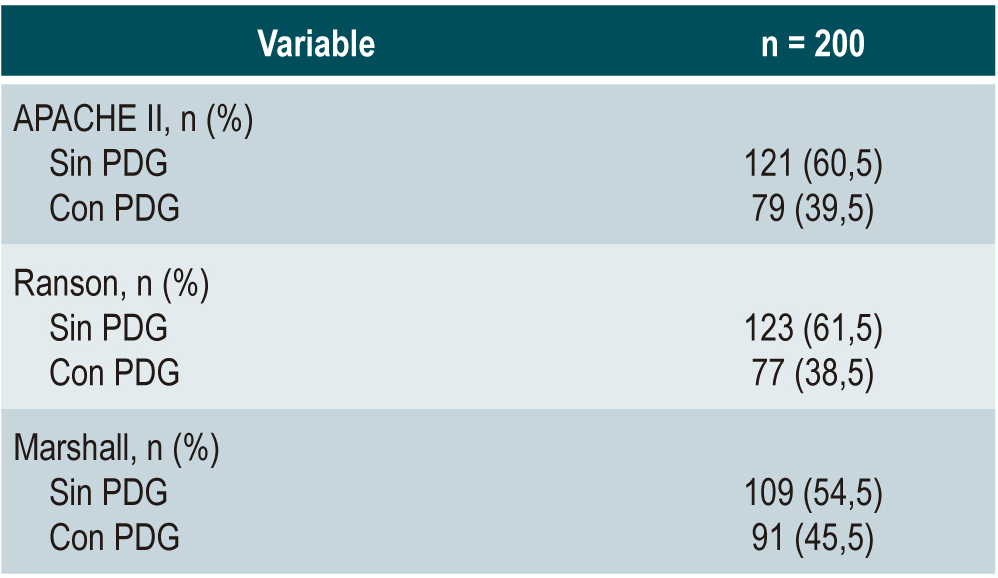
Materials and methods: Two hundred patients between 18 and 65 years old, diagnosed with acute pancreatitis, were evaluated and treated at the Hospital Universitario San Ignacio, Bogotá (Colombia). Three risk scales were used for the estimations. Scores ≥ 8 in the APACHE II system, ≥ 2 in the Modified Marshall Score, or 3 or more positive Ranson criteria were classified as pancreatitis with severity prognostic marker. Agreement between the results was determined using the Kappa coefficient.
Results: According to the Marshall score, 45.5% of the cases were pancreatitis with predicted severity, while APACHE II and Ranson yielded scores of 39.5% and 38.5%, respectively. The Kappa coefficient showed weak agreement between APACHE II and Ranson (Kappa=0.201; 95%CI 0.05-0.34), poor agreement between Ranson and Marshall (Kappa=0.18; 95%CI 0.04-0.32), and moderate agreement between APACHE II and Marshall (Kappa=0.42; 95%CI 0.28-0.56).
Conclusions: There is poor agreement between the pancreatitis severity scoring systems used in Colombia, so they cannot be interpreted as clinically equivalent. The data from this study demonstrate the need to validate the scales in Colombia and Latin America. They also suggest that the Marshall scale overestimates the risk in cities above 2,000 m.a.s.l.
Downloads
References
Huerta-Mercado J. Tratamiento médico de la pancreatitis aguda. Rev Med Hered. 2013;24(3):231-236.
https://doi.org/10.20453/rmh.v24i3.320
Larvin M, McMahon MJ. APACHE-II score for assessment and monitoring of acute pancreatitis. Lancet. 1989;2(8656):201-205.
http://doi.org/10.1016/s0140-6736(89)90381-4
Ranson JH, Spencer FC. Prevention, diagnosis, and treatment of pancreatic abscess. Surgery. 1977;82(1):99-106.
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS; Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62(1):102-11.
http://doi.org/10.1136/gutjnl-2012-302779
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-174. http://doi.org/10.2307/2529310
Werner J, Feuerbach S, Uhl W, Büchler MW. Management of acute pancreatitis: from surgery to interventional intensive care. Gut. 2005;54(3):426-436.
http://doi.org/10.1136/gut.2003.035907
Everhart J. Pancreatitis. In: The burden of digestive diseases in the United States. US Department of Health and Human Services. 2004. p. 119-122.
Wu BU, Johannes RS, Sun X, Tabak Y, Conwell DL, Banks PA. The early prediction of mortality in acute pancreatitis: a large population-based study. Gut. 2008;57(12):1698-1703.
http://doi.org/10.1136/gut.2008.152702
Ponce-Monar CR. Concordancia que existe entre tres escalas de predictores de severidad en pancreatitis aguda en pacientes atendidos en el servicio de medicina interna en el Hospital María Auxiliadora en el periodo 2016. Lima: Universidad Privada San Juan Bautista; 2017.
Rosas FM, Gaxiola WR, Ibáñez GO, Vargas TE, Meza VM, Calvo IJ. Evaluación de las escalas y factores pronóstico en pancreatitis aguda grave. Cir Gen. 2005;27(2):137-143.
Altman DG, Vergouwe Y, Royston P, Moons KG. Prognosis and prognostic research: validating a prognostic model. BMJ. 2009;338:b605.
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














