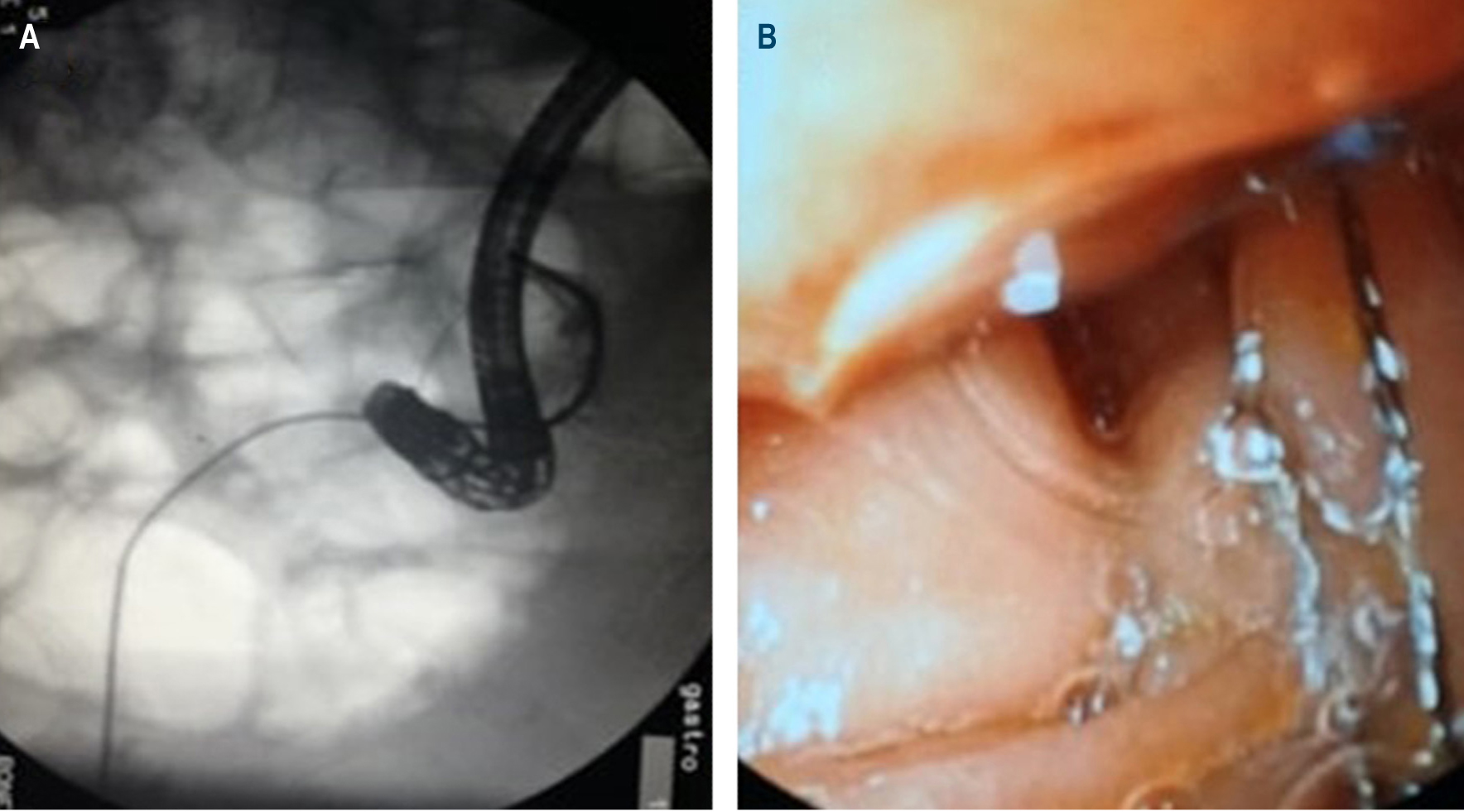
Treatment of choledocholithiasis by ERCP, and instrumentation through a T-tube
DOI:
https://doi.org/10.22516/25007440.385Keywords:
Choledocholithiasis, Endoscopic Retrograde Cholangiopancreatography (ERCP), Bile duct exploration, Kehr tube, Laparoscopic, T-tubeAbstract
The treatment of choledocholithiasis has evolved significantly since Robert Abbé performed the first bile duct exploration via choledochotomy in New York in 1889. Endoscopic retrograde cholangiopancreatography (ERCP), which was initially used for diagnosis, is now only valid as a therapeutic tool. Currently, the main diagnostic methods are magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound (EUS). The treatment of choledocholithiasis moved from the open surgery in which biliary stenting was routinely performed on a Kehr tube or T-tube, to the endoscopic technique using ERCP, sphincteroplasty and instrumentation with balloons and baskets. Additional techniques are now available such as mechanical or extra-corporeal lithotripsy, endoscopic papillary large balloon dilation and SpyGlass cholangioscopy. The laparoscopic technique has been used for several years in different parts of the world for the treatment of choledocholithiasis. Recent studies even propose performing the primary closure of the bile duct or choledochoduodenostomy, so that the T-tube is not necessary. However, in many other places, and for a variety of reasons, open exploratory surgery and the T-tube continue to be used, being an important option in the treatment of some patients.
Case presentation: 88-year-old male patient with recurrent choledocholithiasis and a giant gallstone that was difficult to treat endoscopically, with sepsis of biliary origin, which required open surgical drainage at the emergency room. Choledocotomy was performed, and a T-tube was inserted at the site. Subsequently, a successful joint treatment was performed by the General Surgery Service and the Gastroenterology Service, using T-tube instrumentation and ERCP, respectively.
Downloads
References
Bansal VK, Misra MC, Rajan K, Kilambi R, Kumar S, Krishna A, Kumar A, Pandav CS, Subramaniam R, Arora MK, Garg PK. Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with concomitant gallbladder stones and common bile duct stones: a randomized controlled trial. Surg Endosc. 2014;28(3):875-85.
http://doi.org/10.1007/s00464-013-3237-4
Ding G, Cai W, Qin M. Single-stage vs. two-stage management for concomitant gallstones and common bile duct stones: a prospective randomized trial with long-term follow-up. J Gastrointest Surg. 2014;18(5):947-951. http://doi.org/10.1007/s11605-014-2467-7
Hungness ES, Soper NJ. Management of common bile duct stones. J Gastrointest Surg. 2006;10(4):612-619.
http://doi.org/10.1016/j.gassur.2005.08.015
Xiao LK, Xiang JF, Wu K, Fu X, Zheng MY, Song XX, Xie W. The reasonable drainage option after laparoscopic common bile duct exploration for the treatment of choledocholithiasis. Clin Res Hepatol Gastroenterol. 2018;42(6):564-569.
http://doi.org/10.1016/j.clinre.2018.07.005
Xu Y, Dong C, Ma K, Long F, Jiang K, Shao P, Liang R, Wang L. Spontaneously removed biliary stent drainage versus T-tube drainage after laparoscopic common bile duct exploration. Medicine (Baltimore). 2016;95(39):e5011. http://doi.org/10.1097/MD.0000000000005011
Yin Z, Xu K, Sun J, Zhang J, Xiao Z, Wang J, Niu H, Zhao Q, Lin S, Li Y. Is the end of the T-tube drainage era in laparoscopic choledochotomy for common bile duct stones is coming? A systematic review and meta-analysis. Ann Surg. 2013;257(1):54-66.
http://doi.org/10.1097/SLA.0b013e318268314b
Costi R, Gnocchi A, Di Mario F, Sarli L. Diagnosis and management of choledocholithiasis in the golden age of imaging, endoscopy and laparoscopy. World J Gastroenterol. 2014;20(37):13382-13401.
http://doi.org/10.3748/wjg.v20.i37.13382
Everhart JE, Khare M, Hill M, Maurer KR. Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology. 1999;117(3):632-639.
http://doi.org/10.1016/s0016-5085(99)70456-7
Dasari BV, Tan CJ, Gurusamy KS, Martin DJ, Kirk G, McKie L, Diamond T, Taylor MA. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev. 2013;(9):CD003327.
http://doi.org/10.1002/14651858.CD003327.pub3
Verbesey JE, Birkett DH. Common bile duct exploration for choledocholithiasis. Surg Clin North Am. 2008;88(6):1315-28.
http://doi.org/10.1016/j.suc.2008.08.002
Restrepo C, Sierra S, Penagos S, Palacios OG, Mendoza MC. Manejo sincrónico de la colecistocoledocolitiasis, ¿seguro? Rev Colomb Cir. 2014;29(3):197-203.
Clayton ES, Connor S, Alexakis N, Leandros E. Meta-analysis of endoscopy and surgery versus surgery alone for common bile duct stones with the gallbladder in situ. Br J Surg. 2006;93(10):1185-1191.
http://doi.org/10.1002/bjs.5568
Rogers SJ, Cello JP, Horn JK, Siperstein AE, Schecter WP, Campbell AR, Mackersie RC, Rodas A, Kreuwel HT, Harris HW. Prospective randomized trial of LC+LCBDE vs ERCP/S+LC for common bile duct stone disease. Arch Surg. 2010;145(1):28-33.
http://doi.org/10.1001/archsurg.2009.226
Berggren U, Gordh T, Grama D, Haglund U, Rastad J, Arvidsson D. Laparoscopic versus open cholecystectomy: hospitalization, sick leave, analgesia and trauma responses. Br J Surg. 1994;81(9):1362-1365.
http://doi.org/10.1002/bjs.1800810936
Williams JA, Treacy PJ, Sidey P, Worthley CS, Townsend NC, Russell EA. Primary duct closure versus T-tube drainage following exploration of the common bile duct. Aust N Z J Surg. 1994;64(12):823-826.
http://doi.org/10.1111/j.1445-2197.1994.tb04556.x
Palermo M, Giménez M, Álvarez F, Ortega A, Bruno M, Tarsitano FJ. Abordaje transfistular para el tratamiento de la litiasis residual de la vía biliar. Acta Gastroenterol Latinoam. 2010;40(3):239-243.
Martínez D, Parra P, Díaz D, Lorente JM. Exploración laparoscópica de la vía biliar y coledocorrafia sobre prótesis biliar: dejando atrás el tubo de Kehr. Rev Esp Enferm. 2013;105(3):125-130.
http://dx.doi.org/10.4321/S1130-01082013000300002
Gurusamy KS, Koti R, Davidson BR. T-tube drainage versus primary closure after laparoscopic common bile duct exploration. Cochrane Database Syst Rev. 2013;(6):CD005641.
http://doi.org/10.1002/14651858.CD005641.pub3
Liu JG, Wang YJ, Shu GM, Lou C, Zhang J, Du Z. Laparoscopic versus endoscopic management of choledocholithiasis in patients undergoing laparoscopic cholecystectomy: a meta-analysis. J Laparoendosc Adv Surg Tech A. 2014;24(5):287-294.
http://doi.org/10.1089/lap.2013.0546
Senthilnathan P, Sharma D, Sabnis SC, Srivatsan Gurumurthy S, Senthil Anand E, Nalankilli VP, Anand Vijai N, Praveen Raj P, Parthasarathy R, Rajapandian S, Palanivelu C. Laparoscopic choledochoduodenostomy as a reliable rescue procedure for complicated bile duct stones. Surg Endosc. 2018;32(4):1828-1833.
http://doi.org/10.1007/s00464-017-5868-3
Anwar S, Rahim R, Agwunobi A, Bancewicz J. The role of ERCP in management of retained bile duct stones after laparoscopic cholecystectomy. N Z Med J. 2004;117(1203):U1102.
Gómez M, Gutiérrez O, Jaramillo M. Manejo del cálculo difícil en la vía biliar: serie de casos. Rev Col Gastroenterol. 2015;30(4):461-468.
https://doi.org/10.22516/25007440.10
Classen M, Demling L. Endoskopische Sphinkterotomie der Papilla Vateri und Steinextraktion aus dem Ductus choledochus. Dtsch Med Wochenschr 1974;99(11): 496-497. https://doi.org/10.1055/s-0028-1107790
Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y. Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc. 1974;20(4):148-151.
http://doi.org/10.1016/s0016-5107(74)73914-1
Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57(2):156-159.
http://doi.org/10.1067/mge.2003.52
Cavina E, Franceschi M, Sidoti F, Goletti O, Buccianti P, Chiarugi M. Laparo-endoscopic “rendezvous”: a new technique in the choledocholithiasis treatment. Hepatogastroenterology. 1998;45(23):1430-1435.
Mazzariello R. Tratamiento instrumental postoperatorio de la patología biliar no litiásica. Rev Arg Cir. 1978;34:21-25.
Mazzariello RM. Transcholecystic extraction of residual calculi in common bile duct. Surgery. 1974;75(3):338-347.
Odabasi M, Yildiz MK, Abuoglu HH, Eris C, Ozkan E, Gunay E, Aktekin A, Muftuoglu MT. A modified Rendezvous ERCP technique in duodenal diverticulum. World J Gastrointest Endosc. 2013;5(11):568-73.
http://doi.org/10.4253/wjge.v5.i11.568
Lee JH, Kim HW, Kang DH, Choi CW, Park SB, Kim SH, Jeon UB. Usefulness of percutaneous transhepatic cholangioscopic lithotomy for removal of difficult common bile duct stones. Clin Endosc. 2013;46(1):65-70.
http://doi.org/10.5946/ce.2013.46.1.65
Meek J, Fletcher S, Crumley K, Culp WC, Meek M. Percutaneous rendezvous technique for the management of a bile duct injury. Radiol Case Rep. 2017;13(1):175-178. http://doi.org/10.1016/j.radcr.2017.11.004
Garzón MA, Hernández G, Pérez O, Martínez JD, Molano JC, Marulanda JC, Lizarazo JI, Hormaza N, Rey MH. Factores asociados con el uso de litotripsia mecánica en pacientes con cálculos gigantes de la vía biliar: ¿puede la dilatación papilar con balón grande disminuir su requerimiento? Rev Col Gastroenterol. 2017;32(3):202-208. http://doi.org/10.22516/25007440.151
Staritz M, Ewe K, Meyer zum Büschenfelde KH. Endoscopic papillary dilatation: an alternative to papillotomy? Dtsch Med Wochenschr. 1982;107(23):895-897. http://doi.org/10.1055/s-2008-1070041
Disario JA, Freeman ML, Bjorkman DJ, Macmathuna P, Petersen BT, Jaffe PE, Morales TG, Hixson LJ, Sherman S, Lehman GA, Jamal MM, Al-Kawas FH, Khandelwal M, Moore JP, Derfus GA, Jamidar PA, Ramirez FC, Ryan ME, Woods KL, Carr-Locke DL, Alder SC. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Gastroenterology. 2004;127(5):1291-9. http://doi.org/10.1053/j.gastro.2004.07.017
ASGE Standards of Practice Committee, Maple JT, Ikenberry SO, Anderson MA, Appalaneni V, Decker GA, Early D, Evans JA, Fanelli RD, Fisher D, Fisher L, Fukami N, Hwang JH, Jain R, Jue T, Khan K, Krinsky ML, Malpas P, Ben-Menachem T, Sharaf RN, Dominitz JA. The role of endoscopy in the management of choledocholithiasis. Gastrointest Endosc. 2011;74(4):731-44.
http://doi.org/10.1016/j.gie.2011.04.012
García VA, Zárate AM, Corral A, Pérez A. Manejo actual de la coledocolitiasis. Rev Med Hosp Gen Mex. 1999;62(2):121-127.
Jeong SU, Moon SH, Kim MH. Endoscopic papillary balloon dilation: revival of the old technique. World J Gastroenterol. 2013;19(45):8258-8268.
http://doi.org/10.3748/wjg.v19.i45.8258
Espinoza J, Aliaga M, Rodríguez J, Miraval E, Zegarra A, Bravo E, Prochazka R. Esfinterotomía seguida de dilatación con balón de gran tamaño en el manejo de coledocolitiasis. Eficacia y seguridad en un hospital de Lima-Perú. Rev Gastroenterol Perú. 2016;36(3):203-208.
Marín L, Vera A, Gómez A, Cervera Z, Dávalos M, Alva E, Palacios F, Díaz R, Guzmán E, García G. Dilatación con balón de gran diámetro en el manejo de coledocolitiasis de difícil extracción: experiencia clínica. Rev Gastroenterol Perú. 2016;36(4):330-335.
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














