Actinic colitis of cecal location. Number of cases
DOI:
https://doi.org/10.22516/25007440.366Keywords:
Colitis, radiotherapy, gastrointestinal bleedingAbstract
By definition, actinic colitis includes inflammatory changes of the colorectal mucosa secondary to radiation therapy of nearby tissue. The most frequent location is the rectum, and the most common indication for radiation therapy is a pelvic region neoplasm in the rectum, prostate or cervix. It is estimated that up to half of patients receiving pelvic radiation go on to develop associated gastrointestinal symptoms.
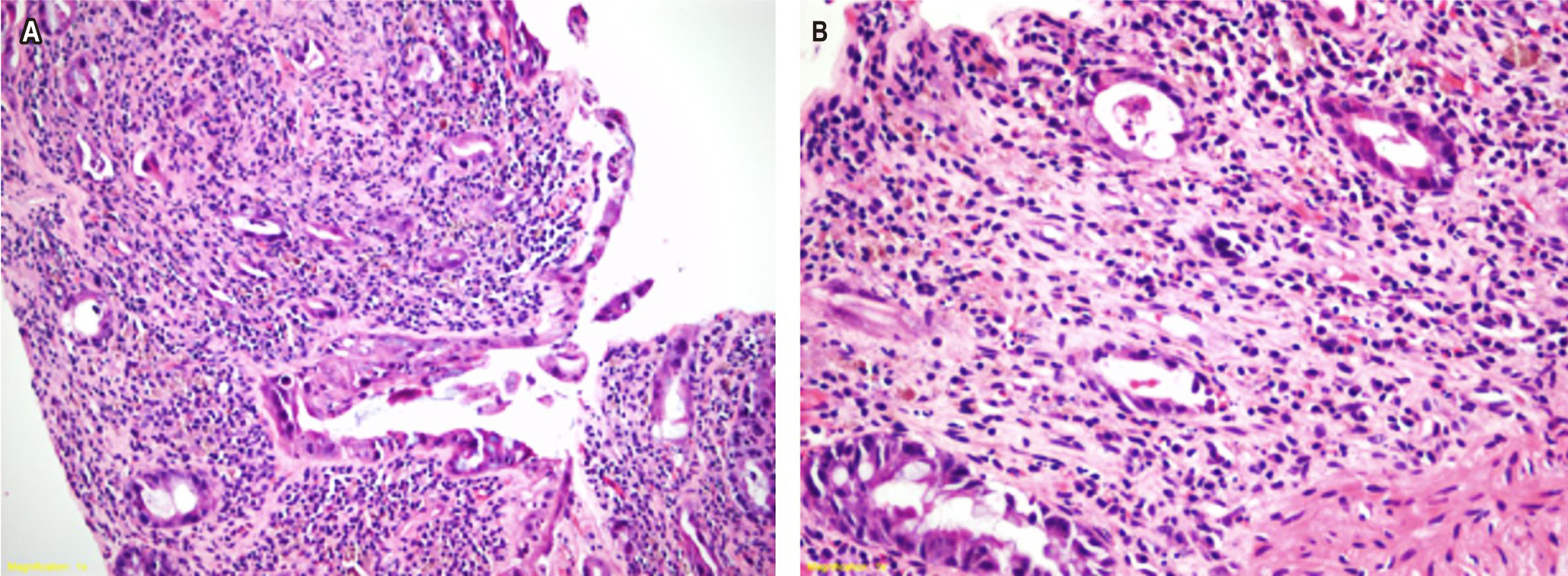
We present two patients with sacroiliac and pelvic bone metastases secondary to prostate adenocarcinoma who received radiation in the lumbosacral and pelvic region. Both patients developed bloody stools soon after radiation therapy. Colonoscopy showed erythema and ulceration, and histopathology found a pattern of ischemic colitis with nucleus and cytomegalovirus infection, fibrous stroma with reactive changes and abundant inflammatory infiltration of neutrophils. These findings are characteristic of acute actinic colitis, but the cecal location has not been reported frequently. Nevertheless, the pelvic location of the cecum and the terminal ileum puts these anatomical segments at risk from the direct impact of radiation therapy. In the acute phase, this condition, is self-limiting and usually resolves with support measures. It is essential that the personnel involved in the management of these patients be aware of this entity and its possible differential diagnoses.
Downloads
References
Qadeer M, Vargo J. Approaches to the prevention and management of radiation colitis. Curr Gastroenterol Rep. 2008;10(5):507-13.
https://doi.org/10.1007/s11894-008-0093-9
Kennedy, G. Heise C. Radiation colitis and proctitis. Clin Colon Rectal Surg. 2007;20(1):64-72.
https://doi.org/10.1055/s-2007-970202
Sarin A, Safar B. Management of radiation proctitis. Gastroenterol Clin N Am. 2013;42(4):913-25.
https://doi.org/10.1016/j.gtc.2013.08.004
Leupin N, Curschmann J, Kranzbühler H, Maurer CA, Laissue JA, Mazzucchelli L. Acute radiation colitis in patients treated with short-term preoperative radiotherapy for rectal cancer. Am J Surg Pathol. 2002;26(4):498-504. https://doi.org/10.1097/00000478-200204000-00013
Theis VS, Sripadam R, Ramani V, Lal S. Chronic radiation enteritis. Clin Oncol (R Coll Radiol). 2010;22(1):70-83. https://doi.org/10.1016/j.clon.2009.10.003
Sinkó, D, Baranyai Z, Nemeskéri C, Teknos D, Jósa V, Hegedus L MA. Symptoms, diagnosis and treatment of radiation-induced enteritis Orv Hetil. 2010;151(36):1450-4.
https://doi.org/10.1556/OH.2010.28939
Kennedy GD, Heise CP. Radiation colitis and proctitis. Clin Colon Rectal Surg. 2007;20:64-72.
https://doi.org/10.1055/s-2007-970202.
Mollà M, Biete A, Piqué J, Panés J. Lesiones intestinales de la radioterapia. Gastroenterol Hepatol. 2001;24(9):454-60. https://doi.org/10.1016/S0210-5705(01)79002-4
Peter R McNally. GI/Liver Plus, Secrets Plus. Colitis: pseudomembranous, microscopic, and radiation. 4.a edición. Elsevier; 2010. p. 349-54. https://doi.org/10.1016/B978-0-323-06397-5.00050-2.
Kountouras J, Zavos C. Recent advances in the management of radiation colitis. World J Gastroenterol. 2008;14(48):7289-301.
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














