Diagnostic performance of the British Society of Gastroenterology predictive criteria for the diagnosis of choledocholithiasis in a Colombian population
DOI:
https://doi.org/10.22516/25007440.365Keywords:
Choledocholithiasis, Diagnostic performance, Predictors, Guidelines, ERCPAbstract
Introduction: Choledocholithiasis (CDL) may be difficult to diagnose. The relevance of making a timely diagnosis lies in its potential negative effects and the fact that treatment requires performing endoscopic retrograde cholangiopancreatography (ERCP), which is a procedure with a high risk of complications. Several guidelines have been proposed for its diagnosis, including the ASGE Guidelines, which are the most widely used although they do not have an ideal performance, and the guidelines recently published by the BSG. The objective of this study was to compare the performance of both guidelines.
Materials and methods: Prospective study carried out between August 1, 2017, and July 31, 2018.
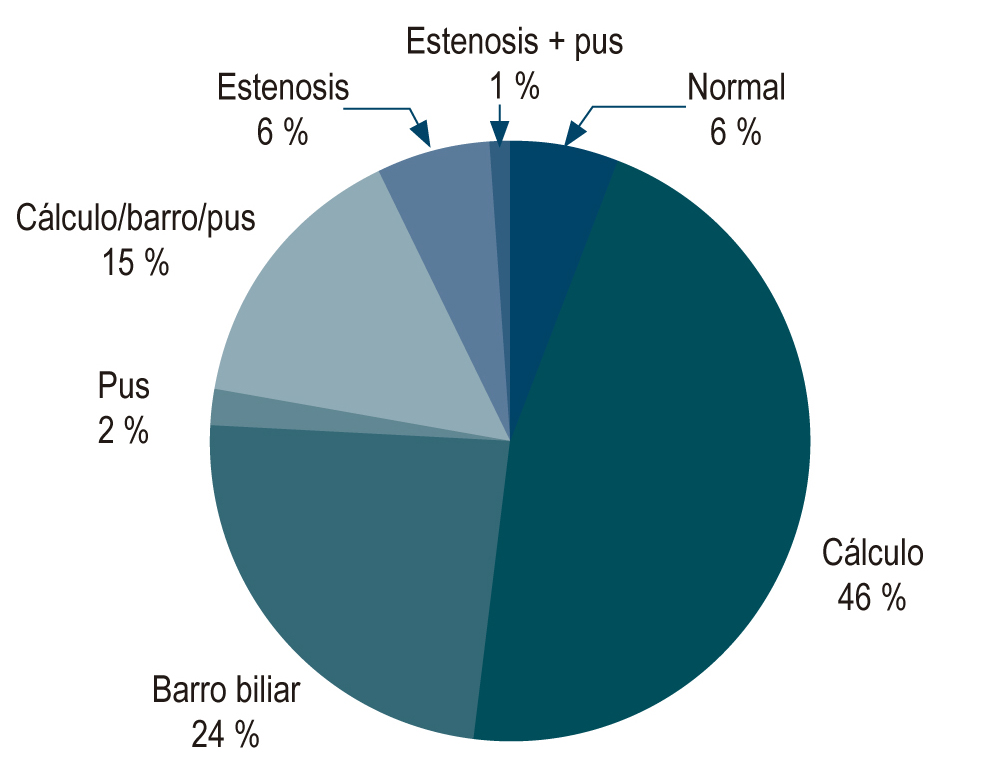
Results: 300 patients were included for analysis. 145 underwent ERCP and choledocholithiasis was confirmed in 124 of them (85.5%). Median AST and ALT levels were higher in patients with choledocholithiasis (207 mg/dL and 290 mg/dL). The rate of post-ERCP complications was 5.5%. Multivariate analysis found no significant association for any predictor of CDL. Regarding the “high probability” score, the BSG guidelines had sensitivity of 65% and specificity of 33%, while the ASGE guidelines had sensitivity of 74% and specificity of 28%. Both guidelines were less efficient for “intermediate probability”.
Conclusions: The ASGE and BSG criteria do not perform well in the population studied to determine whether they had CDL. The ASGE guidelines had a better overall performance than the BSG guidelines.
Downloads
References
European Association for the Study of the Liver (EASL). Electronic address: easloffice@easloffice.eu. EASL Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016;65(1):146-181.
http://doi.org/10.1016/j.jhep.2016.03.005
Csendes A, Diaz JC, Burdiles P, Maluenda F, Morales E. Risk factors and classification of acute suppurative cholangitis. Br J Surg. 1992;79(7):655-8.
http://doi.org/10.1002/bjs.1800790720
Yang MH, Chen TH, Wang SE, Tsai YF, Su CH, Wu CW, Lui WY, Shyr YM. Biochemical predictors for absence of common bile duct stones in patients undergoing laparoscopic cholecystectomy. Surg Endosc. 2008;22(7):1620-4.
http://doi.org/10.1007/s00464-007-9665-2
Costi R, Sarli L, Caruso G, Iusco D, Gobbi S, Violi V, Roncoroni L. Preoperative ultrasonographic assessment of the number and size of gallbladder stones: is it a useful predictor of asymptomatic choledochal lithiasis? J Ultrasound Med. 2002;21(9):971-6.
http://doi.org/10.7863/jum.2002.21.9.971
Anderson MA, Fisher L, Jain R, Evans JA, Appalaneni V, Ben Menachem T, Cash BD, Anton G, Early DS, Fanelli RD, Fisher DA, Fukami N, Ha Hwang J, Ikenberry SO, Jue TL, Khan KM, Krinsky ML, Malpas PM, Maple JT, Sharaf RN, Shergill AK, Dominitz JA. Complications of ERCP. Gastrointest Endosc. 2012;75(3):467-473.
http://doi.org/10.1016/j.gie.2011.07.010
Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, Dinelli M, Minoli G, Crosta C, Comin U, Fertitta A, Prada A, Passoni GR, Testoni PA. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001;96(2):417-23.
http://doi.org/10.1111/j.1572-0241.2001.03594.x
ASGE Standards of Practice Committee, Maple JT, Ben-Menachem T, Anderson MA, Appalaneni V, Banerjee S, Cash BD, Fisher L, Harrison ME, Fanelli RD, Fukami N, Ikenberry SO, Jain R, Khan K, Krinsky ML, Strohmeyer L, Dominitz JA. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. 2010;71(1):1-9.
http://doi.org/10.1016/j.gie.2009.09.041
Williams E, Beckingham I, El Sayed G, Gurusamy K, Sturgess R, Webster G, Young T. Updated guideline on the management of common bile duct stones (CBDS). Gut. 2017;66(5):765-782.
http://doi.org/10.1136/gutjnl-2016-312317
Adams MA, Hosmer AE, Wamsteker EJ, Anderson MA, Elta GH, Kubiliun NM, Kwon RS, Piraka CR, Scheiman JM, Waljee AK, Hussain HK, Elmunzer BJ. Predicting the likelihood of a persistent bile duct stone in patients with suspected choledocholithiasis: accuracy of existing guidelines and the impact of laboratory trends. Gastrointest Endosc. 2015;82(1):88-93.
http://doi.org/10.1016/j.gie.2014.12.023
Sethi S, Wang F, Korson AS, Krishnan S, Berzin TM, Chuttani R, Pleskow DK, Sawhney MS. Prospective assessment of consensus criteria for evaluation of patients with suspected choledocholithiasis. Dig Endosc. 2016;28(1):75-82.
http://doi.org/10.1111/den.12506
Vargas RD, Córdoba CP, Uriza LF, Costa V, Mosquera-Klinger G, Ortega DA. Concordancia entre los hallazgos por colangiopancreatografía por resonancia magnética y los hallazgos por colangiopancreatografía endoscópica retrograda en pacientes hospitalizados por enfermedad biliar litiásica en el Hospital Universitario San Ignacio (Bogotá-Colombia) entre los años 2005 a 2011. Rev Gastroenterol. 2015;35(3):226-230.
Gómez M, Pion J, Otero W. Predictores de coledocolitiasis en pacientes sometidos a colangiografía retrógrada endoscópica en el Hospital El Tunal de Bogotá. Rev Col Gastroenterol. 2011;26(4):243-252.
Jurgaky JM. Prevalencia y factores de riesgo de elevación de transaminasas en pacientes con coledocolitiasis. Bogotá: Universidad Nacional de Colombia; 2017.
Rubin MI, Thosani NC, Tanikella R, Wolf DS, Fallon MB, Lukens FJ. Endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis: testing the current guidelines. Dig Liver Dis. 2013;45(9):744-9.
http://doi.org/10.1016/j.dld.2013.02.005
Magalhães J, Rosa B, Cotter J. Endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis: From guidelines to clinical practice. World J Gastrointest Endosc. 2015;7(2):128-34.
http://doi.org/10.4253/wjge.v7.i2.128
Adams MA, Hosmer AE, Wamsteker EJ, Anderson MA, Elta GH, Kubiliun NM, Kwon RS, Piraka CR, Scheiman JM, Waljee AK, Hussain HK, Elmunzer BJ. Predicting the likelihood of a persistent bile duct stone in patients with suspected choledocholithiasis: accuracy of existing guidelines and the impact of laboratory trends. Gastrointest Endosc. 2015;82(1):88-93.
http://doi.org/10.1016/j.gie.2014.12.023
Narváez-Rivera RM, González-González JA, Monreal-Robles R, García-Compean D, Paz-Delgadillo J, Garza-Galindo AA, Maldonado-Garza HJ. Accuracy of ASGE criteria for the prediction of choledocholithiasis. Rev Esp Enfer. 2016;108(6):309-314.
http://doi.org/10.17235/reed.2016.4212/2016
Benites HE, Palacios FV, Asencios JL, Aguilas R, Segovia NS. Rendimiento de los criterios predictivos de la ASGE en el diagnóstico de coledocolitiasis en el Hospital Edgardo Rebagliati Martins. Rev Gastroenterol. 2017;37(2):111-119.
Ebrahim M, Sorensen LT, Jorgensen LN, Kalaitzakis E. Current clinical algorithms for predicting common bile duct stones have only moderate accuracy. Dig Endosc. 2018;30(4):477-484.
http://doi.org/10.1111/den.12994
Nathwani RA, Kumar SR, Reynolds TB, Kaplowitz N. Marked elevation in serum transaminases: an atypical presentation of choledocholithiasis. Am J Gastroenterol. 2005;100(2):295-298.
http://doi.org/10.1111/j.1572-0241.2005.40793.x
Tozatti J, Mello AL, Frazon O. Predictor factors for choledocholithiasis. Arq Bras Cir Dig. 2015;28(2):109-112.
http://doi.org/10.1590/S0102-67202015000200006
Bourgouin S, Truchet X, Lamblin G, De Roulhac J, Platel JP, Balandraud P. Dynamic analysis of commonly used biochemical parameters to predict common bile duct stones in patients undergoing laparoscopic cholecystectomy. Surg Endosc. 2017;31(11):4725-4734.
http://doi.org/10.1007/s00464-017-5549-2
Stepien M, Fedirko V, Duarte-Salles T, Ferrari P, Freisling H, Trepo E, Trichopoulou A, Bamia C, Weiderpass E, Olsen A, Tjønneland A, Overvad K, Boutron-Ruault MC, Fagherazzi G, Racine A, Kühn T, Kaaks R, Aleksandrova K, Boeing H, Lagiou P, Benetou V, Trichopoulos D, Palli D, Grioni S, Tumino R, Naccarati A, Panico S, Bueno-de-Mesquita HB, Peeters PH, Lund E, Quirós JR, Nápoles OC, Sánchez MJ, Dorronsoro M, Huerta JM, Ardanaz E, Ohlsson B, Sjöberg K, Werner M, Nystrom H, Khaw KT, Key TJ, Gunter M, Cross A, Riboli E, Romieu I, Jenab M. Prospective association of liver function biomarkers with development of hepatobiliary cancers. Cancer Epidemiol. 2016;40:179-87.
http://doi.org/10.1016/j.canep.2016.01.002
Woo YS, Lee KH, Lee KT, Lee JK, Kim JM, Kwon CHD, Joh JW, Kang D, Cho J. Postoperative changes of liver enzymes can distinguish between biliary stricture and graft rejection after living donor liver transplantation: A longitudinal study. Medicine (Baltimore). 2017;96(40):e6892.
http://doi.org/10.1097/MD.0000000000006892
Perales SR, Souza LRMF, Crema E. comparative evaluation of magnetic resonance cholangiopancreatography and perioperative cholangiography in patients with suspect choledocholithiasis. Arq Bras Cir Dig. 2019;32(1):e1416.
http://doi.org/10.1590/0102-672020180001e1416
Makmun D, Fauzi A, Shatri H. Sensitivity and Specificity of Magnetic Resonance Cholangiopancreatography versus Endoscopic Ultrasonography against Endoscopic Retrograde Cholangiopancreatography in Diagnosing Choledocholithiasis: The Indonesian Experience. Clin Endosc. 2017;50(5):486-490.
http://doi.org/10.5946/ce.2016.159
Meeralam Y, Al-Shammari K, Yaghoobi M. Diagnostic accuracy of EUS compared with MRCP in detecting choledocholithiasis: a meta-analysis of diagnostic test accuracy in head-to-head studies. Gastrointest Endosc. 2017;86(6):986-993.
http://doi.org/10.1016/j.gie.2017.06.009
Suárez AL, LaBarre NT, Cotton PB, Payne KM, Coté GA, Elmunzer BJ. An assessment of existing risk stratification guidelines for the evaluation of patients with suspected choledocholithiasis. Surg Endosc. 2016;30(10):4613-4618.
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |















