Intestinal lipomatosis: Report of two cases
DOI:
https://doi.org/10.22516/25007440.288Keywords:
Lipomatosis, gastrointestinal, gastrointestinal diseases, endoscopy, double ballon enteroscopy, colonoscopyAbstract
Intestinal lipomatosis is a proliferation of histologically normal fatty tissue in the gastrointestinal tract. It is characterized benign, asymptomatic, slow growing tumors with sub-epithelial origins. On rare occasions, they become symptomatic and can be associated with major complications such as gastrointestinal obstructions and bleeding. This rare pathology has been reported several times in the literature but not in Colombia prior to this study. We present two cases that were evaluated and followed up at the Unión de Cirujanos SAS and the University of Caldas in Manizales, Colombia.
The first is a 70-year-old man who had a history of colic associated with bloating and postprandial diarrhea. The initial upper digestive endoscopy reported multiple yellowish, submucosal lesions in the duodenum. His histological diagnosis was lipomas. In this case, an endoscopic video capsule determined the distribution and characteristics of the lesions throughout the gastrointestinal tract and assessed complications.
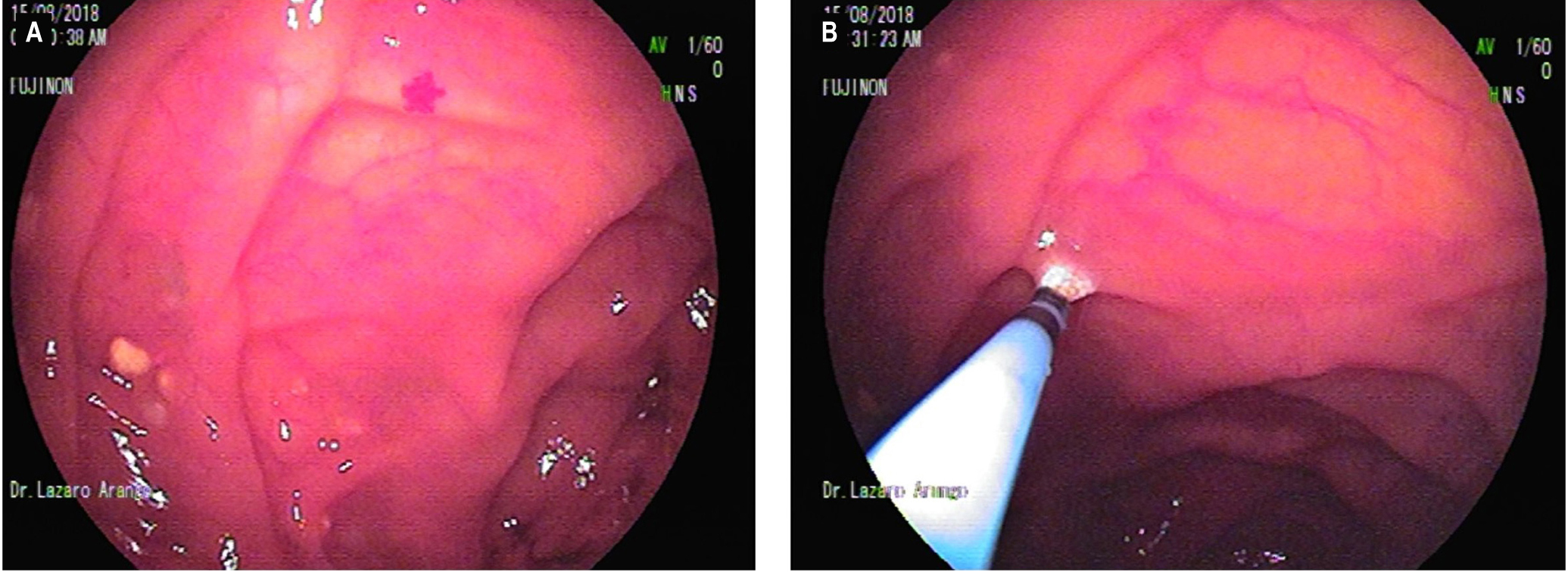
The second is an 81-year-old man who entered the institution due to lipothymia and rectal bleeding. Upper endoscopy and colonoscopy were normal, but a videocapsule endoscopy showed lipomatous lesions one of which was bleeding and had adjacent angiodysplasia. He was treated with double balloon enteroscopy and Argon plasma therapy.
Downloads
References
Zirpe D, Wani M, Tiwari P, Ramaswamy PK, Kumar RP. Duodenal Lipomatosis as a Curious Cause of Upper Gastrointestinal Bleed: A Report with Review of Literature. J Clin Diagn Res. 2016;10(5):PE01‐PE4.
http://doi.org/10.7860/JCDR/2016/19851.7881
Komagata T, Takebayashi S, Hirasawa K, Fukawa T, Arai M. Extensive lipomatosis of the small bowel and mesentery: CT and MRI findings. Radiat Med. 2007;25(9):480‐483. http://doi.org/10.1007/s11604-007-0162-2
Krachman MS, Dave PB, Gumaste VV. Bleeding duodenal lipoma. J Clin Gastroenterol. 1992;15(2):180‐181.
Kumar K, Noori MR, Patel KM, Yuen W, Bello C. Rare diagnosis of intestinal lipomatosis complicated by intussusception in an adult: A case report. Int J Surg Case Rep. 2017;39:339‐342.
http://doi.org/10.1016/j.ijscr.2017.08.038
Fang SH, Dong DJ, Chen FH, Jin M, Zhong BS. Small intestinal lipomas: diagnostic value of multi-slice CT enterography. World J Gastroenterol. 2010;16(21):2677‐2681. http://doi.org/10.3748/wjg.v16.i21.2677
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |















