Todani Type I Common Bile Duct Cyst in an Adult Patient: Clinical Case and Literature Review
DOI:
https://doi.org/10.22516/25007440.1074Keywords:
Common bile duct cyst, common bile duct, abdominal pain, Roux-en-Y anastomosis, case reportsAbstract
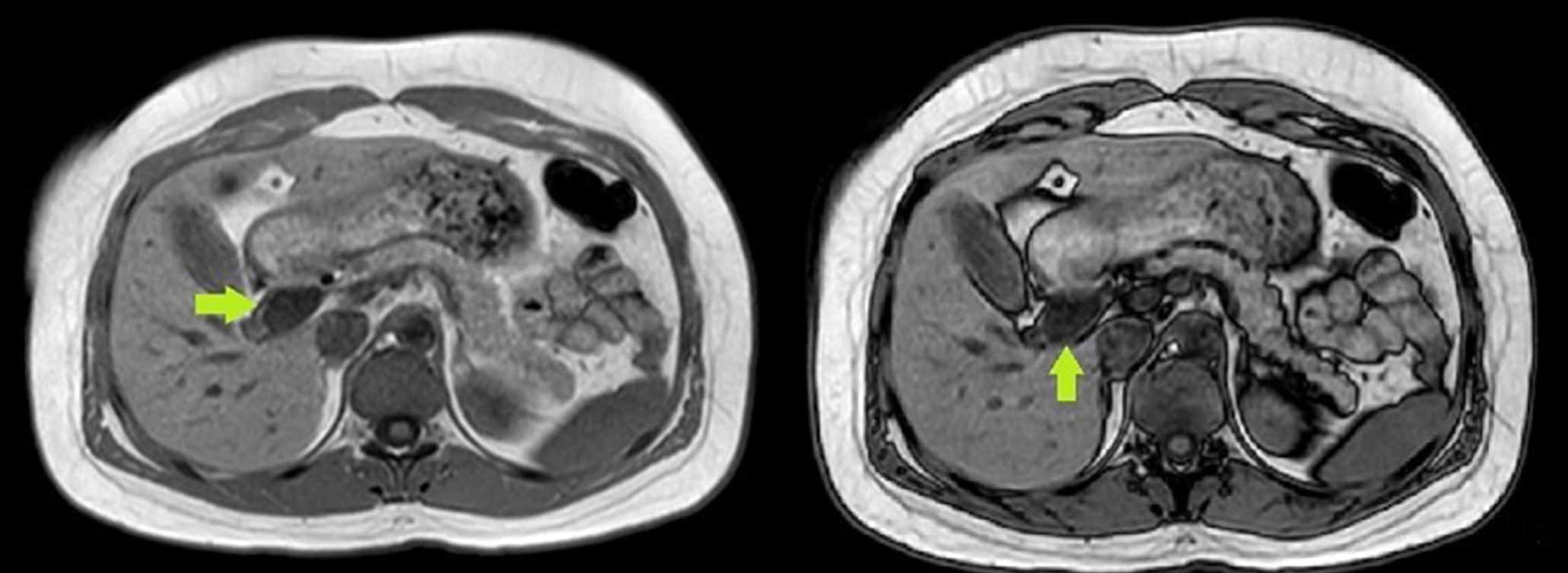
Bile duct cysts are characterized by intrahepatic or extrahepatic bile duct dilation. It is a rare congenital pathology, diagnosed mainly in children. The clinical manifestation in adults is usually nonspecific but essential due to their increased risk of developing carcinoma. We present the case of a 37-year-old female patient who consulted for pain in the epigastrium radiating to the right hypochondrium, associated with emesis and choluria. The hepatobiliary ultrasound was normal, but due to the risk of choledocholithiasis, a magnetic resonance cholangiopancreatography was performed, revealing a cystic dilation of the proximal common bile duct of approximately 2 cm, classified as Todani type I. Bile duct cysts have been associated with several complications, and cholangiocarcinoma is the most important. The probability of malignancy is higher in adults and Todani type I cysts.
Downloads
References
Baison GN, Bonds MM, Helton WS, Kozarek RA. Choledochal cysts: Similarities and differences between Asian and Western countries. World J Gastroenterol. 2019;25(26):3334-3343. https://doi.org/10.3748/wjg.v25.i26.3334
Farías-Molina SM, Castillo-Machado RL, Sanhueza-Palma NC, Calzadilla-Riveras JA. Quiste de colédoco Todani tipo II: caso clínico y revisión. Medwave. 2016;16(9):e6583. https://doi.org/10.5867/medwave.2016.09.6583
Yamaguchi M. Congenital choledochal cyst. Analysis of 1,433 patients in the Japanese literature. Am J Surg, 1980;140(5):653-657. https://doi.org/10.1016/0002-9610(80)90051-3
Bhavsar MS, Vora HB, Giriyappa VH. Choledochal cysts: a review of literature. Saudi J Gastroenterol. 2012;18(4):230-236. https://doi.org/10.4103/1319-3767.98425
Honnavara-Srinivasan P, Anbalagan A, Shanmugasundaram R, Obla Lakshmanamoorthy N. Management of Choledochal Cysts at a Tertiary Care Centre: A Nine-Year Experience from India. Surg Res Pract. 2020;2020:8017460. https://doi.org/10.1155/2020/8017460
Moslim MA, Takahashi H, Seifarth FG, Walsh RM, Morris-Stiff G. Choledochal Cyst Disease in a Western Center: A 30-Year Experience. J Gastrointest Surg. 2016;20(8):1453-1463. https://doi.org/10.1007/s11605-016-3181-4
Babbitt DP. Congenital choledochal cysts: new etiological concept based on anomalous relationships of the common bile duct and pancreatic bulb. Ann Radiol (Paris). 1969:12(3):231-240.
Sánchez JA, Gómez S, Morales C, Hoyos SI. Quistes del colédoco. Rev Colomb Cir. 2015;30(4):296-305. https://doi.org/10.30944/20117582.379
Miron A, Popa LG, Toma EA, Calu V, Parvuletu RF, Enciu O. The Curious Case of the Choledochal Cyst-Revisiting the Todani Classification: Case Report and Review of the Literature. Diagnostics (Basel). 2023;13(6):1059. https://10.3390/diagnostics13061059
Ye Y, Lui VCH, Tam PKH. Pathogenesis of Choledochal Cyst: Insights from Genomics and Transcriptomics. Genes (Basel). 2022;13(6):1030. https://doi.org/10.3390/genes13061030
Kumar M, Rajagopalan S. Choledochal cyst. Med J Armed Forces India. 2012;68(3):296-298. https://doi.org/10.1016/j.mjafi.2012.04.011
Marcos A. Diagnóstico prenatal de quiste de colédoco: presentación de un caso. Rev Argent Ultrason. 2008;7(1):53-56.
Alonso-Lej F, Rever WB, Pessagno DJ. Congenital choledochal cyst, with a report of 2, and an analysis of 94, cases. Int Abstr Surg. 1959;108(1):1-30.
Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134(2):263-269. https://doi.org/10.1016/0002-9610(77)90359-2
Sureka B, Rastogi A, Bihari C, Bharathy KGS, Sood V, Alam S. Imaging in ductal plate malformations. Indian J Radiol Imaging. 2017;27(1):6-12. https://doi.org/10.4103/0971-3026.202966
Sosa R, Hernández E, López A, Bolaños J, González F. Diagnóstico y Tratamiento del Quiste del Colédoco Neonatal. Reporte de Casos. Rev Guatem Cir. 2016;22(1):25-28.
Tannuri AC, Hara LA, Paganoti GF, Andrade WC, Tannuri U. Choledochal cysts in children: How to Diagnose and Operate on. Clinics (Sao Paulo). 2020;75:e1539. https://doi.org/10.6061/clinics/2020/e1539
Machado NO, Chopra PJ, Al-Zadjali A, Younas S. Choledochal Cyst in Adults: Etiopathogenesis, Presentation, Management, and Outcome-Case Series and Review. Gastroenterol Res Pract. 2015;2015:602591. https://doi.org/10.1155/2015/602591
Pandit N, Deo KB, Yadav TN, Gautam S, Dhakal Y, Awale L, et al. Choledochal Cyst: A Retrospective Study of 30 Cases From Nepal. Cureus. 2020;12(11):e11414. https://doi.org/10.7759/cureus.11414
Talini C, DE-Carvalho BC, Antunes LA, Schulz C, Sabbaga CC, Andrade SG, et al. Choledochal cyst in the pediatric population: experience of 13 laparoscopic procedures in two years at a single institution. Rev Col Bras Cir. 2018;10;45(3):e1854. https://doi.org/10.1590/0100-6991e-20181854
Arroyo-Martínez L, Montero-Carvajal R, Ayi-Wong J. Quiste del colédoco como causa de dolor abdominal: revisión de un caso y bibliografía. Acta Med Costarric. 2004;46(3):149-151. https://doi.org/10.51481/amc.v46i3.150
Søreide K, Søreide JA. Bile duct cyst as precursor to biliary tract cancer. Ann Surg Oncol. 2007;14(3):1200-11. https://doi.org/10.1245/s10434-006-9294-3
Cención JD, Chanis R; Méndez J. Características clínicas y demográficas de los pacientes con quiste de colédoco atendidos en el Hospital del Niño Dr. José R. Esquivel en Panamá durante los años 2005 a 2018. Pediátr Panamá. 2019;48(2):4-10. https://doi.org/10.37980/im.journal.rspp.20191574
Monteiro VV, Pinheiro F, Costa K, Seixas Z, Da Silva R. Choledochal cyst- unusual presentation in the adult phase: Case report. Int J Surg Case Rep. 2020;70:33-36. https://doi.org/10.1016/j.ijscr.2020.03.014
Singham J, Schaeffer D, Yoshida E, Scudamore C. Choledochal cysts: analysis of disease pattern and optimal treatment in adult and paediatric patients. HPB (Oxford). 2007;9(5):383-387. https://doi.org/10.1080/13651820701646198
Tello de Meneses A, Riggen L, Orozco E. Quiste de colédoco tipo I: Diagnóstico por imagen y anastomosis hepático-duodenal como medida terapéutica. Bol Med Hosp Infant Mex. 2013;70(6):482-487.
Lourenço AL, Proença A, Gil P.A Rare Case of Todani Type-III Choledochal Cyst. Acta Radiologica Portuguesa. 2020;32(2):23-25. https://doi.org/10.25748/arp.19632
Sacher VY, Davis JS, Sleeman D, Casillas J. Role of magnetic resonance cholangiopancreatography in diagnosing choledochal cysts: Case series and review. World J Radiol. 2013;5(8):304-312. https://doi.org/10.4329/wjr.v5.i8.304
Katabathina VS, Kapalczynski W, Dasyam AK, Anaya-Baez V, Menias CO. Adult choledochal cysts: current update on classification, pathogenesis, and cross-sectional imaging findings. Abdom Imaging. 2015;40(6):1971-1981. https://doi.org/10.1007/s00261-014-0344-1
Lewis VA, Adam SZ, Nikolaidis P, Wood C, Wu JG, Yaghmai V, et al. Imaging of choledochal cysts. Abdom Imaging. 2015;40(6):1567-80. https://doi.org/10.1007/s00261-015-0381-4
Gyawali S, Adhikari G, Shrestha S, Pradhan S, Bhandari RS. Concomitant hilar cholangiocarcinoma with choledochal cyst and cholelithiasis in an asymptomatic patient: A case report. Int J Surg Case Rep. 2021;84:106094. https://doi.org/10.1016/j.ijscr.2021.106094
López-Ruiz R, Aguilera-Alonso D, Muñoz-Aguilar G, Fonseca-Martín R. Quistes de colédoco, una causa inusual de ictericia en pediatría. Presentación de serie de casos. Rev Chil Pediatr. 2016;87(2):137-142. https://doi.org/10.1016/j.rchipe.2015.08.009
Ten-Hove A, Meijer VE, Hulscher BF, de Kleine HJ. Meta-analysis of risk of developing malignancy in congenital choledochal malformation. Br J Surg. 2018;105(5):482-490. https://doi.org/10.1002/bjs.10798
Gadelhak N, Shehta A, Hamed H. Diagnosis and management of choledochal cyst: 20 years of single center experience. World J Gastroenterol. 2014;20(22):7061-7066. https://doi.org/10.3748/wjg.v20.i22.7061
Ouaïssi M, Kianmanesh R, Belghiti J, Ragot E, Mentha G, Adham M, et al. Todani Type II Congenital Bile Duct Cyst: European Multicenter Study of the French Surgical Association and Literature Review. Ann Surg. 2015;262(1):130-8. https://doi.org/10.1097/SLA.0000000000000761
Calderón M, Abarzúa J, Quiroga C, Gana J, de Barbieri F. Coledococele: caso diagnosticado por resonancia magnética. Rev Chil Radiol. 2020;26(2):76-78. http://dx.doi.org/10.4067/S0717-93082020000200076
Liu Y, Sun J, Guo S, Liu Z, Zhu M, Zhang ZL. The distal classification and management of choledochal cyst in adults: Based on the relation between cyst and pancreatic duct. Medicine (Baltimore). 2017;96(12):e6350. https://doi.org/10.1097/MD.0000000000006350
Vargas-Vásquez N, Jiménez-Luna G, Quiñones J, Sánchez-Temoche C. Enfermedad de Caroli: a propósito de un caso. Revista. colomb. Gastroenterol.. 2020;35(3):390-393. https://doi.org/10.22516/25007440.387
Zhen C, Xia Z, Long L, Lishuang M, Pu Y, Wenjuan Z, et al. Laparoscopic excision versus open excision for the treatment of choledochal cysts: a systematic review and meta-analysis. Int Surg. 2015;100(1):115-122. https://doi.org/10.9738/INTSURG-D-14-00165.1
Liu Y, Yao X, Li S, Liu W, Liu L, Liu J. Comparison of therapeutic effects of laparoscopic and open operation for congenital choledochal cysts in adults. Gastroenterol Res Pract. 2014;2014:670260. https://doi.org/10.1155/2014/670260
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |