Self-expanding Metal Stents in Malignant Obstruction of the Esophagus: A 25-Year Multicentric Study
DOI:
https://doi.org/10.22516/25007440.1064Keywords:
esophageal cancer, Metal stent, Dysphagia, PalliationAbstract
Background: Self-expanding metal prostheses improve dysphagia in patients with incurable esophageal cancer (EC). New stents have been introduced, and chemoradiotherapy has been implemented for EC, changing patients’ risk profiles. It is unknown whether this has affected palliation with stents.
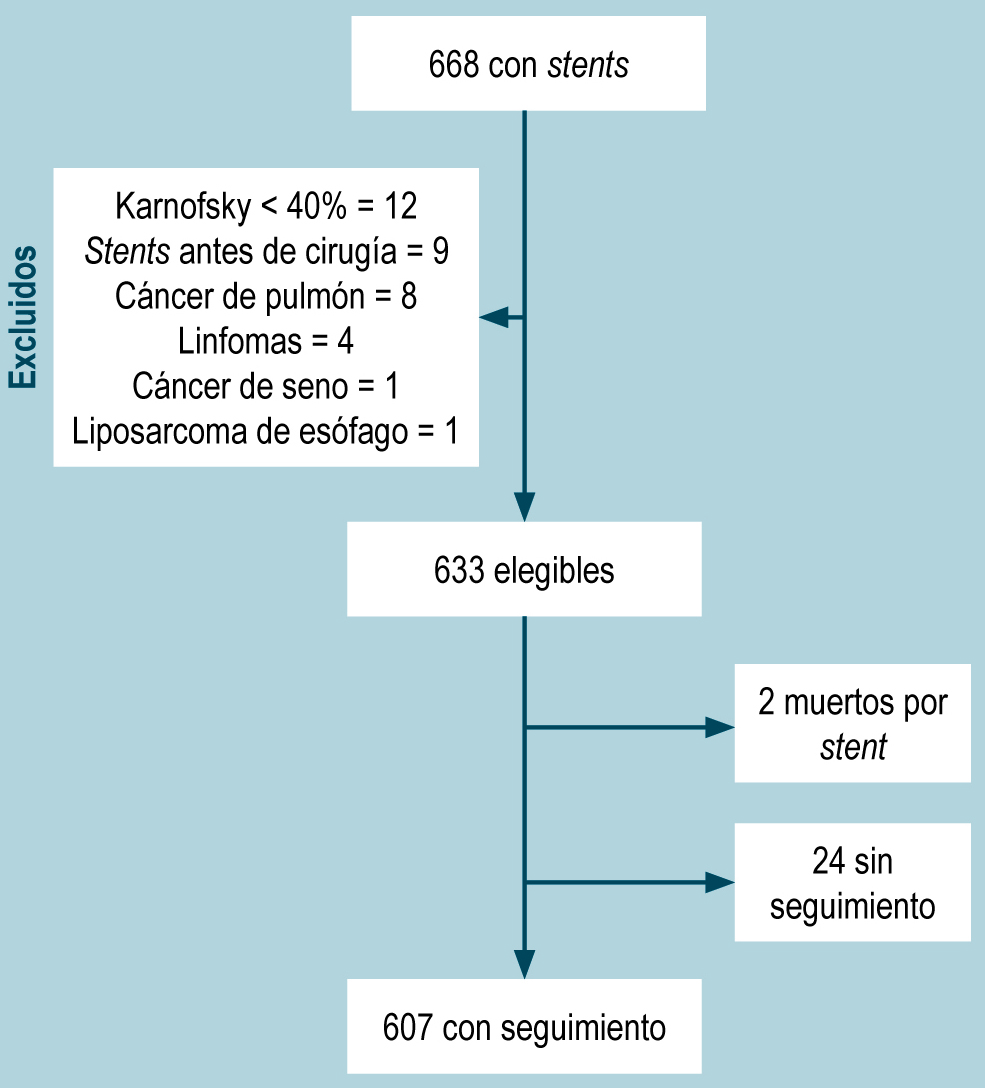
Patients and methods: Retrospective study in three centers in Medellín-Colombia; patients undergoing placement of palliative esophageal prostheses for malignant dysphagia (1997-2022). Major and minor complications after implantation, the influence of oncological therapies, and survival were evaluated for 1997-2009 (n = 289) and 2010-2022 (n = 318).
Results: 607 patients underwent esophageal prostheses; 296 (48.8%) became complicated. It was higher in the second period (52.5% vs. 48.1%), as were major complications (20.8% vs. 14.2%, p = 0.033), with no differences in minor complications (33.9% vs 31.8%, p = 0.765). Also, 190 (31.3%) patients presented with recurrent dysphagia, stable in both periods. Migration increased over time (from 13.1% to 18.2%, p = 0.09). The most common minor adverse event was pain, increasing over time (from 24.9% to 33.95%, p < 0.01), and associated factors were chemoradiotherapy, absence of fistula, and squamous cell carcinoma. Acid reflux decreased in the second group (p = 0.038). Twelve percent of patients required another intervention for feeding. Survival was not impacted by time and use of stents.
Conclusions: Stents are an alternative in non-surgical malignant dysphagia, although recurrent dysphagia has not decreased over time. Minor stent-related complications are increasing in association with the implementation of chemoradiotherapy.
Downloads
References
WCRF International. Oesophageal Cancer Statistics | World Cancer Research Fund International [Internet]. WCRF International. 2022 [consultado el 16 de julio de 2022]. Disponible en: https://www.wcrf.org/cancer-trends/oesophageal-cancer-statistics/
Morgan E, Soerjomataram I, Rumgay H, Coleman HG, Thrift AP, Vignat J, et al. The global landscape of esophageal squamous cell carcinoma and esophageal adenocarcinoma incidence and mortality in 2020 and projections to 2040: New estimates from GLOBOCAN 2020. Gastroenterology. 2022;163(3):649-658.e2. https://doi.org/10.1053/j.gastro.2022.05.054
Homs MYV, Steyerberg EW, Eijkenboom WMH, Tilanus HW, Stalpers LJA, Bartelsman JFWM, et al. [Palliative treatment of esophageal cancer with dysphagia: more favourable outcome from single-dose internal brachytherapy than from the placement of a self-expanding stent; a multicenter randomised study]. Ned Tijdschr Geneeskd. 2005;149(50):2800-6.
Spaander MCW, Baron TH, Siersema PD, Fuccio L, Schumacher B, Escorsell À, et al. Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48(10):939-48. https://doi.org/10.1055/s-0042-114210
Celestin LR. Permanent intubation in inoperable cancer of the oesophagus and cardia: a new tube. Ann R Coll Surg Engl. 1959;25(2):165-70.
Valbuena JV, Olarte H. Prótesis per oral endoscópica en el tratamiento de cáncer de esófago y cardias. Rev Col Gastroenterol. 1987;2(1):17-22.
Castaño R, Sanín E, Ruiz MH. Stent esofágico de nitinol en el manejo de las fístulas esofagorrespiratorias malignas. Rev Col Gastroenterol. 2003;18(2):78-82.
Jackson CE, Johnson LS, Williams DA, Laasch HU, Edwards DW, Harvey AG, et al. A viewpoint on material and design considerations for oesophageal stents with extended lifetime Invited Viewpoint. J Mater Sci. 2022;57:3-26. https://doi.org/10.1007/s10853-021-06700-9
Castaño R. Técnicas en stents gastrointestinales endoscópicos: cómo, cuándo, manejo de complicaciones, selección del stent y costos. Rev Col Gastroenterol. 2012;27(1):32-44.
Castaño R, Ruiz Vélez MH, Juliao Baños F, Sanín Fonnegra E, Álvarez Barrera O, Lopera Bonilla J. Eficacia de un nuevo stent de nitinol fabricado localmente, en el tratamiento de la obstrucción maligna esofágica. Rev Col Gastroenterol. 2003;18(4):211-21.
Castaño R, Álvarez O, Lopera J, Ruiz MH, Juliao F, Sanín E, et al. Endoprótesis metálicas autoexpandibles en la obstrucción maligna esofágica y gastroduodenal. Rev Col Cirugía. 2005;20(1):33-48.
Castaño R, Álvarez O, Lopera J, Ruiz MH, Rojas A, Álvarez A, et al. Development and implementation of a new nitinol stent design for managing benign stenoses and fistulas of the digestive tract. Rev Col Gastroenterol. 2015;30(3):261-72. https://doi.org/10.22516/25007440.49
Yang Z, Wu Q, Wang F, Ye X, Qi X, Fan D. A Systematic Review and Meta-Analysis of Randomized Trials and Prospective Studies Comparing Covered and Bare Self-Expandable Metal Stents for the Treatment of Malignant Obstruction in the Digestive Tract. International Journal of Medical Sciences. 2013;10(7):825-35. https://doi.org/10.7150/ijms.5969
Hussain Z, Diamantopoulos A, Krokidis M, Katsanos K. Double-layered covered stent for the treatment of malignant oesophageal obstructions: Systematic review and meta-analysis. World J Gastroenterol. 2016;22(34):7841-50. https://doi.org/10.3748/wjg.v22.i34.7841
Law R, Prabhu A, Fujii-Lau L, Shannon C, Singh S. Stent migration following endoscopic suture fixation of esophageal self-expandable metal stents: a systematic review and meta-analysis. Surg Endosc. 2018;32(2):675-81. https://doi.org/10.1007/s00464-017-5720-9
Zhao CL, Gu B, Huo XB, Xia FF. I-125 seed-loaded versus normal stent insertion for obstructive esophageal cancer: a meta-analysis. Videosurgery and other Miniinvasive Techniques. 2021;16(4):633-40. https://doi.org/10.5114/wiitm.2021.104205
Ogilvie AL, Dronfield MW, Ferguson R, Atkinson M. Palliative intubation of oesophagogastric neoplasms at fibreoptic endoscopy. Gut. 1982;23(12):1060-7. https://doi.org/10.1136/gut.23.12.1060
Kumar S, Bahdi F, Emelogu IK, Yu AC, Coronel M, Ge PS, et al. How much progress have we made?: a 20-year experience regarding esophageal stents for the palliation of malignant dysphagia. Dis Esophagus. 2022;35(6):doab085. https://doi.org/10.1093/dote/doab085
Chandan S, Mohan BP, Khan SR, Bhogal N, Canakis A, Bilal M, et al. Clinical efficacy and safety of palliative esophageal stenting without fluoroscopy: a systematic review and meta-analysis. Endosc Int Open [Internet]. 2020 [consultado el 6 de mayo de 2023];8(7):E944. Disponible en: /pmc/articles/PMC7297607/
Moutzoukis M, Argyriou K, Kapsoritakis A, Christodoulou D. Endoscopic luminal stenting: Current applications and future perspectives. World J Gastrointest Endosc [Internet]. 2023 [consultado el 6 de mayo de 2023];15(4):195–215. Disponible en: https://pubmed-ncbi-nlm-nih-gov.udea.lookproxy.com/37138934/
Johnson LA, Marino KA, Muesse J. Esophageal Stenting: Expert Techniques. CTSNet; 2022. https://doi.org/10.25373/ctsnet.19224678
Ivanov AI, Popov VA, Burmistrov MV. Complications of endoscopic esophageal stent implantation. Kazan Med J. 2021;102(1):74-84. https://doi.org/10.17816/KMJ2021-74
Tinusz B, Soós A, Hegyi P, Sarlós P, Szapáry L, Erős A, et al. Efficacy and safety of stenting and additional oncological treatment versus stenting alone in unresectable esophageal cancer: A meta-analysis and systematic review. Radiotherapy and Oncology. 2020;147:169-77. https://doi.org/10.1016/j.radonc.2020.05.015
Schiemer M, Bettinger D, Mueller J, Schultheiss M, Schwacha H, Hasselblatt P, et al. Reduction of esophageal stent migration rate with a novel over-the-scope fixation device (with video). Gastrointest Endosc. 2022;96(1):1-8. https://doi.org/10.1016/j.gie.2022.02.001
Martins B da C, Retes FA, Medrado BF, de Lima MS, Pennacchi CMPS, Kawaguti FS, et al. Endoscopic management and prevention of migrated esophageal stents. World J Gastrointest Endosc. 2014;6(2):49-54. https://doi.org/10.4253/wjge.v6.i2.49
Reijm AN, Didden P, Bruno MJ, Spaander MCW. Early pain detection and management after esophageal metal stent placement in incurable cancer patients: A prospective observational cohort study. Endosc Int Open. 2016;04(08):E890-4. https://doi.org/10.1055/s-0042-111202
Castaño R, Álvarez O, Lopera J, Ruiz MH, Rojas A, Álvarez A, et al. Desarrollo e implementación de un nuevo diseño de stent de nitinol para el manejo de estenosis y fístulas benignas del tracto digestivo. Rev Colomb Gastroenterol. 2015;30(3):261-72. https://doi.org/10.22516/25007440.49
Fuccio L, Scagliarini M, Frazzoni L, Battaglia G. Development of a prediction model of adverse events after stent placement for esophageal cancer. Gastrointest Endosc. 2016;83(4):746-52. https://doi.org/10.1016/j.gie.2015.08.047
Gao F, Xu YL, Liu YJ, Sun MH. Outcomes of self-expandable metal stent placement for malignant oesophageal strictures. Clin Radiol. 2020;75(2):156.e21-156.e27. https://doi.org/10.1016/j.crad.2019.10.008
Spaander MCW, van der Bogt RD, Baron TH, Albers D, Blero D, de Ceglie A, et al. Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - Update 2021. Endoscopy. 2021;53(7):751-762. https://doi.org/10.1055/a-1475-0063
Yang ZM, Geng HT, Wu H. Radioactive Stent for Malignant Esophageal Obstruction: A Meta-Analysis of Randomized Controlled Trials. J Laparoendosc Adv Surg Tech A [Internet]. 2021 [consultado el 14 de diciembre de 2023];31(7):783–9. Available from: https://pubmed.ncbi.nlm.nih.gov/32915105/
Zhu HD, Guo JH, Mao AW, Lv WF, Ji JS, Wang WH, et al. Conventional stents versus stents loaded with (125)iodine seeds for the treatment of unresectable oesophageal cancer: a multicentre, randomised phase 3 trial. Lancet Oncol [Internet]. 2014 [consultado el 14 de diciembre de 2023];15(6):612–9. Available from: https://pubmed.ncbi.nlm.nih.gov/24742740/
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |