Dyssynergic Defecation Concerning Proctalgia Fugax: An Observational Study
DOI:
https://doi.org/10.22516/25007440.1033Keywords:
Anorectal disorders, Anorectal manometry, Proctalgia, Dyssynergic defecation, Gastrointestinal diseasesAbstract
Introduction: There is no clarity about manometric findings in patients with proctalgia fugax; evidence shows different results. This study aims to evaluate dyssynergic defecation through anorectal manometry in Colombian patients in two gastroenterology centers in Bogotá, Colombia.
Materials and methods: A cross-sectional descriptive observational study in adult patients with proctalgia fugax undergoing anorectal manometry and treated in two gastroenterology centers in Bogotá between 2018 and 2020.
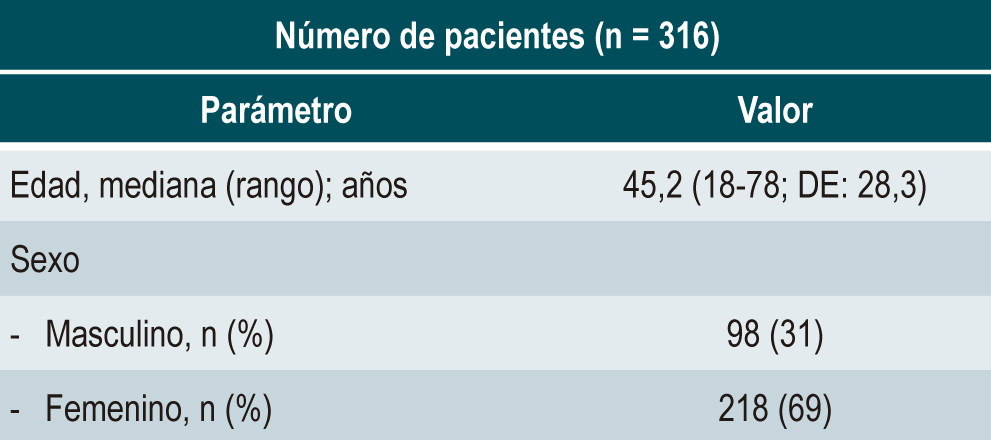
Results: 316 patients were included, predominantly women (65%), with a median age of 45.2 (range: 18-78; standard deviation [SD]: 28.3). Four percent of patients had hypertonicity, 50% were normotonic, and 46% were hypotonic. Regarding manometric parameters, 50% had normal pressure, and 46% had anal sphincter hypotonia; 76% had a normal voluntary contraction test. Dyssynergic defecation was documented in 5% of patients, and the most frequent was type I, followed by type III. A rectoanal inhibitory reflex was identified in all patients, 42% with altered sensory threshold and 70% with abnormal balloon expulsion. There was an agreement between the results of the anorectal manometry and the subjective report of the digital rectal exam by the head nurse who performed the procedure.
Conclusions: The data obtained in the present study suggest that proctalgia is not related to the elevated and sustained basal contracture of the sphincter but neither to the alteration in voluntary contraction since most patients have typical values.
Downloads
References
Drossman DA, Hasler WL. Rome IV - Functional GI disorders: Disorders of gut-brain interaction. Gastroenterology. 2016;150(6):1257-61. https://doi.org/10.1053/j.gastro.2016.03.035
Ciriza De Los Ríos C, Mínguez M, Remes-Troche JM, Lacima G. High-resolution and high-definition anorectal manometry: Rediscovering anorectal function. Rev Esp Enferm Dig. 2018;110(12):794-805. https://doi.org/10.17235/reed.2018.5705/2018
Bjoern MX, Perdawood SK. Manometric assessment of anorectal function after transanal total mesorectal excision. Tech Coloproctol. 2020;24(3):231-6. https://doi.org/10.1007/s10151-020-02147-3
Fox M, Markopoulos K, Flückiger M. Investigations of anorectal function. Ther Umschau. 2021;78(9):513-21. https://doi.org/10.1024/0040-5930/a001304
Rao SSC, Bharucha AE, Chiarioni G, Felt-Bersma R, Knowles C, Malcolm A, et al. Anorectal disorders. Gastroenterology. 2016;150(6):1430-1442.e4. https://doi.org/10.1053/j.gastro.2016.02.009
Ciriza De Los Ríos C, Ruiz De León San Juan A, Díaz-Rubio García M, Tomás Moros E, García Durán F, Muñoz Yagüe T, et al. Diferencias en las presiones del canal anal y la sensibilidad rectal en pacientes con incontinencia anal, estreñimiento crónico y sujetos sanos. Rev Esp Enferm Dig. 2010;102(12):683-90. https://doi.org/10.4321/S1130-01082010001200002
Carrington EV, Heinrich H, Knowles CH, Rao SS, Fox M, Scott SM, et al. Methods of anorectal manometry vary widely in clinical practice: Results from an international survey. Neurogastroenterol Motil. 2017;29(8):e13016. https://doi.org/10.1111/nmo.13016
Nakao A, Okamoto Y, Sunami M, Fujita T, Tsuji T. The oldest patient with gallstone ileus: Report of a case and review of 176 cases in Japan. Kurume Med J. 2008;55(1-2):29-33. https://doi.org/10.2739/kurumemedj.55.29
Meza Madrid D, Hani de Ardila AC, Costa VA, Leguízamo AM, Puentes Leal GA, Ardila Hani AF. Cómo realizar e interpretar una manometría anorrectal de alta resolución. Rev Colomb Gastroenterol. 2019;34(4):404-10. https://doi.org/10.22516/25007440.411
Krogh K, Chiarioni G, Whitehead W. Management of chronic constipation in adults. United Eur Gastroenterol J. 2017;5(4):465-72. https://doi.org/10.1177/2050640616663439
Kitaguchi D, Nishizawa Y, Sasaki T, Tsukada Y, Ito M. Clinical benefit of high-resolution anorectal manometry for the evaluation of anal function after intersphincteric resection. Color Dis. 2019;21(3):335-41. https://doi.org/10.1111/codi.14528
Villarreal AD, Barney VAC, Hani A, Leguizamo AM, Ardila A, Madrid DM. Update of high-resolution anorectal manometry interpretation using the London classification. Rev Colomb Gastroenterol. 2019;34(4):411-5. https://doi.org/10.22516/25007440.484
Cho HM, Kim H, Yoo R, Kim G, Kye BH. Effect of biofeedback therapy during temporary stoma period in rectal cancer patients: A prospective randomized trial. J Clin Med. 2021;10(21):5172. https://doi.org/10.3390/jcm10215172
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














