Endoscopic Ultrasound-guided Hepaticogastrostomy, Experience in Colombia: Case Series
DOI:
https://doi.org/10.22516/25007440.1030Keywords:
Hepaticogastrostomy, Endoscopy, Biliary obstruction, ColombiaAbstract
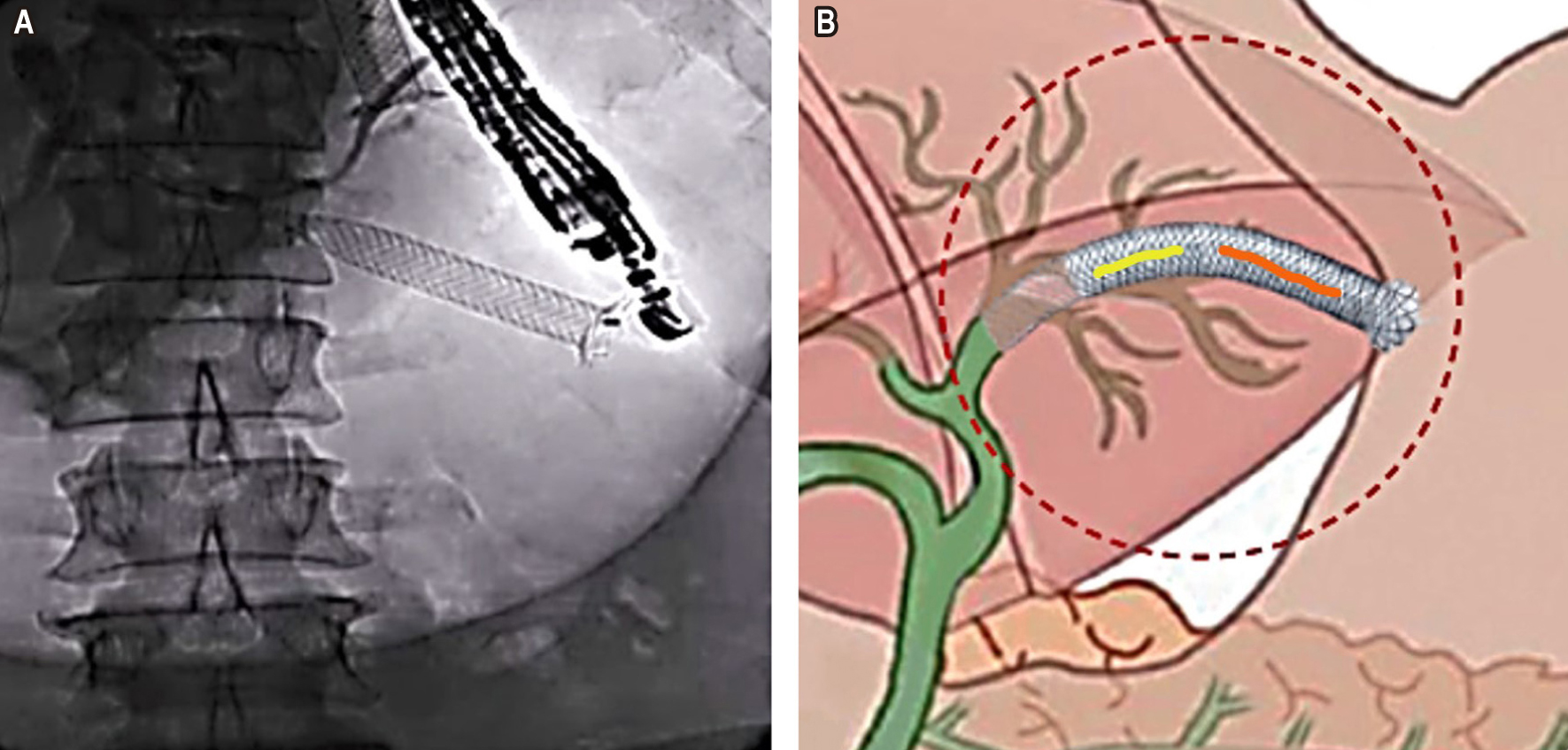
The primary tool for malignant biliary obstruction is decompression of the bile duct, using endoscopic retrograde cholangiopancreatography (ERCP) with stenting, which is satisfactory in many cases; still, the actual challenge arises when it is impossible to cannulate the ampulla of Vater due to neoplastic involvement at that level. Although percutaneous transhepatic biliary drainage (PTBD) is an option, it has high morbidity, which directly impacts the patient’s quality of life by having an external device added to a malignant pathology. With the arrival of endoscopic ultrasound (EUS), new methods have been reported, such as EUS-guided hepaticogastrostomy (EUS-HGS), which is performed through a natural orifice (NOTES) and positively impacts the outcome of these patients. Below is an example of our experience with the first three cases in Colombia.
Downloads
References
Sharaiha RZ, Khan MA, Kamal F, Tyberg A, Tombazzi CR, Ali B, et al. Efficacy and safety of EUS-guided biliary drainage in comparison with percutaneous biliary drainage when ERCP fails: a systematic review and meta-analysis. Gastrointest Endosc. 2017;85(5):904-914. https://doi.org/10.1016/j.gie.2016.12.023
Jirapinyo P, Lee LS. Endoscopic Ultrasound-Guided Pancreatobiliary Endoscopy in Surgically Altered Anatomy. Clin Endosc. 2016;49(6):515‐529. https://doi.org/10.5946/ce.2016.144
Marx M, Caillol F, Sfumato P, Romero J, Ratone JP, Pesenti C, et al. EUS-guided hepaticogastrostomy in the management of malignant biliary obstruction: Experience and learning curve in a tertiary referral center. Dig Liver Dis. 2022;54(9):1236-1242. https://doi.org/10.1016/j.dld.2022.05.008
Nennstiel S, Weber A, Frick G, Haller B, Meining A, Schmid RM, et al. Drainage-related Complications in Percutaneous Transhepatic Biliary Drainage: An Analysis Over 10 Years. J Clin Gastroenterol. 2015;49(9):764-70. https://doi.org/10.1097/MCG.0000000000000275
Oh HC, Lee SK, Lee TY, Kwon S, Lee SS, Seo DW, et al. Analysis of percutaneous transhepatic cholangioscopy-related complications and the risk factors for those complications. Endoscopy. 2007;39(8):731-6. https://doi.org/10.1055/s-2007-966577
Vanella G, Lisotti A. EUS-guided hepaticogastrostomy: Who is the ideal patient, who is the ideal endoscopist? Dig Liver Dis. 2022;54(9):1234-1235. https://doi.org/10.1016/j.dld.2022.06.007
TaeWoong Medical. [Internet]. Niti-S & ComVi Biliary Stent. User’s Manual. [consultado el 1 de junio del 2023]. Disponible en: http://www.taewoongmedical.com/data/bbsData/16481920162.pdf
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














